Translate this page into:
Diagnostic significance of clay-like materials aspirated from thyroid nodules

-
Received: ,
Accepted: ,
How to cite this article: Kanematsu R, Hirokawa M, Suzuki A, Higuchi M, Miyauchi A, Akamizu T. Diagnostic significance of clay-like materials aspirated from thyroid nodules. CytoJournal. 2024;21:17. doi: 10.25259/Cytojournal_89_2023
Abstract
Objective:
The simplest way to determine the adequacy of aspirated materials is the on-site gross visual assessment of aspirated materials. However, few studies have examined the gross findings of thyroid aspirates. This study aimed to clarify the diagnostic significance of clay-like material aspirated from thyroid nodules.
Material and Methods:
We reviewed 69,848 thyroid nodules that underwent aspiration cytology at Kuma Hospital between January 2007 and August 2021. Among them, 355 (0.5%) nodules with aspirated materials described as clay-like materials were retrospectively examined.
Results:
Among 355 nodules, 322 (90.7%) were categorized as cystic fluid or benign. The aspirated materials were mainly composed of non-epithelial components, including colloid or proteinaceous materials, foamy histiocytes, and degenerative red blood cells. In original ultrasound reports, the incidence of intermediate and high suspicion was 11.0%. Malignant cells were observed in 21 nodules (5.9%), one-third of which were papillary thyroid carcinomas. The materials aspirated from papillary and follicular thyroid carcinomas exhibited necrotic carcinoma cells derived from infarcted areas. The overall risk of malignancy was 3.9%. The risk of malignancy in nodules interpreted as highly suspicious on ultrasound examination was 37.5%.
Conclusion:
As clay-like materials aspirated from thyroid nodules were considered sufficient specimens, the recognition contributes to avoiding unnecessary second punctures. The presence of clay-like materials was indicative of the colloid and/or blood components of benign cystic lesions, or, more rarely, of infarcted carcinoma. The ultrasound examination results tended to overestimate nodules. We should reaffirm that on-site gross visual assessment of aspirated materials is a fast and reasonably accurate predictor of the on-site adequacy of the samples.
Keywords
On-site gross visual assessment
Clay-like material
Cystic fluid
Infarction
Risk of malignancy
INTRODUCTION
Fine-needle aspiration cytology (FNAC) has been established as a reliable modality for the pre-operative diagnosis of thyroid nodules. The diagnostic accuracy depends on the methods and techniques of aspiration, smearing, fixation, and staining, as well as the diagnostic skills and experience of cytopathologists. The key factor is obtaining representative samples from targeted thyroid lesions. To reduce the incidence of non-diagnostic samples, several methods, including aspiration with ultrasound guidance,[1,2] rapid on-site evaluation (ROSE),[3,4] and liquid-based cytology (LBC),[5,6] have been performed.
The simplest way to determine the adequacy of aspirated materials is on-site gross visual assessment for aspirated materials.[7-14] A speculative diagnosis is occasionally possible. Honey-like, abscess-like, and watery-clear fluid materials indicate benign thyroid nodules,[15] acute suppurative thyroiditis[16] or anaplastic thyroid carcinoma,[17] and parathyroid cysts,[18] respectively. When aspirates from regional lymph nodes are liquid, metastatic papillary thyroid carcinoma is a possible diagnosis.[19] Ren et al. described that toothpaste-like materials were aspirated from the early stage degenerating thyroid nodules.[20] The materials are reddish-brown in color, three-dimensional, and sticky, giving them the appearance of clay. No detailed study of the aspirate showing its characteristic gross findings had been found. This study aimed to clarify the diagnostic significance of clay-like materials aspirated from thyroid nodules.
MATERIAL AND METHODS
Ethical approval was obtained from the Ethics Committee of our hospital. The study protocol was reviewed and approved by the Institutional Review Board (20200709-1). We reviewed the cytology report database of 69,848 thyroid nodules that underwent FNAC performed by a single pathologist (MHir) at Kuma Hospital from January 2007 to August 2021. Clinical and cytological data were obtained from the medical records of patients at Kuma Hospital. All findings and test results in the electronic medical records (HOPE Cloud Chart, Fujitsu, Tokyo, Japan) and pathology reporting system (CNA-Net, Sakura Finetek Japan Co., Tokyo, Japan) were stored in a data warehouse. We extracted relevant data using a keyword search from the database. Ultrasonography was performed using the APLIO 80 SSA-770A (Toshiba Medical Systems Co., Ltd., Otawara, Japan) or APLIO 500 TUS-A500 (Toshiba) ultrasound machine with PLT-805AT (8 MHz, Toshiba) or PLT-1005BT (10 MHz, Toshiba) probes. Ultrasound-guided Fine-needle aspiration (FNA) was performed using a 22-gauge needle without local anesthesia. The needle was inserted in a plane perpendicular to the scanning plane (perpendicular positioning).[21] Smears were prepared using the press and release method and subsequently stained with Papanicolaou stain. Clay-like materials were defined as reddish brown, sticky, and three-dimensional [Figure 1]. Among the 69,848 nodules, 355 (0.5%) nodules had aspirates described as clay-like materials in the medical records and were retrospectively examined. Ultrasound reports were categorized based on the American Thyroid Association guidelines.[22] The sonographic patterns were classified into high suspicion, intermediate suspicion, low suspicion, very low suspicion, and benign. FNAC results were categorized based on the Japanese System for Reporting Thyroid Cytopathology.[23-26] The diagnostic categories were classified into unsatisfactory, cyst fluid, benign, undetermined significance, follicular neoplasm, suspicious for malignancy, and malignant. The follow-up period ranged from 1 to 14 years (mean 11.2 years).

- Macroscopic finding of clay-like material. It is reddish-brown and looks like clay.
RESULTS
Original ultrasound reports
Table 1 shows the original ultrasound reports of thyroid nodules with clay-like materials. The most frequently classified category was very low suspicion (47.3%), followed by low suspicion (36.3%). The incidence of intermediate and high suspicion was 11.0%. In terms of the total number of nodules, follicular nodular disease, follicular neoplasm, and malignant tumors were suspected in 166 (46.8%), 167 (47.0%), and 46 (13.0%) nodules, respectively. Most (91.3%) nodules suspected to be malignant were papillary thyroid carcinomas.
| Category | Cases (%) | Suspected lesions | |
|---|---|---|---|
| Type | Cases | ||
| Non-classified | 15 (4.2) | ||
| Benign | 4 (1.1) | Cyst | 3 |
| Follicular nodular disease | 1 | ||
| Very low suspicion | 168 (47.3) | Cyst | 4 |
| Calcified nodule | 1 | ||
| Follicular nodular disease or follicular neoplasm | 163 | ||
| Low suspicion | 129 (36.3) | Follicular nodular disease | 2 |
| Follicular nodular disease or follicular neoplasm | 1 | ||
| Neoplasm, unclassified | 115 | ||
| Follicular neoplasm | 3 | ||
| Papillary thyroid carcinoma | 8 | ||
| Intermediate suspicion | 23 (6.5) | Neoplasm, unclassified | 1 |
| Follicular carcinoma | 1 | ||
| Papillary thyroid carcinoma | 20 | ||
| Malignant tumor | 1 | ||
| High suspicion | 16 (4.5) | Papillary thyroid carcinoma | 14 |
| Malignant tumor | 2 | ||
Original cytological reports
All the specimens were considered adequate [Table 2]. Among 355 nodules, 322 (90.7%) were categorized as cyst fluid (124, 34.9%) or benign (198, 55.8%). 14 nodules (3.9%) were reported to be malignant, and half of them were suspected to be papillary thyroid carcinoma.
| Category | Cases (%) | Suspected lesions | |
|---|---|---|---|
| Type | Cases | ||
| Unsatisfactory | 0 (0) | ||
| Cyst fluid | 124 (34.9) | Benign cyst | 124 |
| Benign | 198 (55.8) | Benign lesion | 6 |
| Subacute thyroiditis | 1 | ||
| Follicular nodular disease | 191 | ||
| Undetermined significance | 16 (4.5) | Necrotic cells | 6 |
| Atypical cells | 1 | ||
| Follicular nodular disease or follicular neoplasm | 2 | ||
| Papillary thyroid carcinoma | 7 | ||
| Follicular neoplasm | 3 (0.8) | Follicular neoplasm | 3 |
| Suspicious for malignancy | 0 (0) | ||
| Malignant | 14 (3.9) | Papillary thyroid carcinoma | 7 |
| Poorly differentiated thyroid carcinoma | 1 | ||
| Medullary thyroid carcinoma | 1 | ||
| Anaplastic thyroid carcinoma | 1 | ||
| Adenocarcinoma | 2 | ||
| Squamous cell carcinoma | 2 | ||
Cytological findings
Table 3 shows the cytological findings of thyroid nodules with clay-like materials. The smears were mainly composed of abundant non-epithelial components, including colloid or proteinaceous materials (79.4%), foamy histiocytes (71.8%), and degenerative red blood cells (67.6%), consistent with cystic content and/or blood clots. Calcified materials were observed in 16.9% of the samples, but not in the morphology of psammoma bodies. Few epithelial cells were observed. A few benign follicular cells and squamous cells were present in 47.0% and 6.2% of the nodules, respectively. Malignant cells were observed in 21 nodules (5.9%), 14 of which were papillary thyroid carcinomas associated with necrotic carcinoma cells. Abundant amyloid was present in the medullary carcinoma nodule. The anaplastic carcinoma specimen included a large number of necrotic carcinoma cells and neutrophils.
| Component type | Number of cases (%) |
|---|---|
| Non-cellular components | |
| Colloid or proteinaceous materials | 282 (79.4) |
| Nuclear streaming | 227 (63.9) |
| Calcified materials | 60 (16.9) |
| Cholesterol crystals | 21 (5.9) |
| Oxalate crystals | 13 (3.7) |
| Hematoidin | 6 (1.7) |
| Amyloid | 1 (0.3) |
| Non-epithelial cells | |
| Foamy cells | 255 (71.8) |
| Degenerative red blood cells | 240 (67.6) |
| Multinucleated giant cells | 143 (40.3) |
| Necrotic cells | 44 (12.4) |
| Lymphocytes | 25 (7.0) |
| Neutrophils | 23 (6.5) |
| Epithelial components | |
| Benign follicular cells | 167 (47.0) |
| Benign squamous cells | 22 (6.2) |
| Neoplastic cells | 26 (7.3) |
| Follicular neoplasm | 5 |
| Papillary thyroid carcinoma | 14 |
| Poorly differentiated thyroid carcinoma | 1 |
| Medullary thyroid carcinoma | 1 |
| Anaplastic thyroid carcinoma | 1 |
| Adenocarcinoma, NOS | 2 |
| Squamous cell carcinoma | 2 |
NOS: Not otherwise specified
Re-aspiration
Eleven nodules (3.1%) underwent re-aspiration. The indications were suspicious ultrasound findings (7 nodules), suspicious cytological findings (2 nodules), and information about suspected malignancy from previous physicians (2 nodules). Re-aspiration was identified as benign and malignant in 6 nodules and 1 nodule, respectively. The identification rate of benign and malignant cases was 63.6%.
Pathological findings
Among 355 thyroid nodules, 33 and 321 were surgically resected and followed up, respectively. The findings of the remaining 7 nodules were unknown because the patients were transferred to another hospital. Table 4 shows the pathological diagnoses of the resected nodules. Nineteen (57.6%) and 14 (42.4%) nodules were benign and malignant, respectively. Among the 19 benign lesions, 15 (78.9%) were cystic follicular nodular disease, and the clay-like materials accounted for the cystic contents [Figure 2] and/or blood clots [Figure 3]. Nine (64.3%) of the 14 malignant tumors were papillary thyroid carcinomas. Clay-like materials aspirated from three of nine papillary thyroid carcinomas and two of three follicular thyroid carcinomas [Figures 4 and 5] were necrotic cells derived from the infarcted areas. Those in medullary thyroid carcinoma and anaplastic thyroid carcinoma were consistent with amyloid deposition and abscess-like areas, respectively.
| Lesion type | Pathological diagnosis | Cases |
|---|---|---|
| Benign lesions (19) |
Follicular nodular disease, cystic | 15 |
| Burned out tumor | 2 | |
| Lymphoepithelial cyst | 1 | |
| Follicular adenoma | 1 | |
| Malignant tumors (14) |
Papillary thyroid carcinoma | 9 |
| Follicular thyroid carcinoma | 3 | |
| Medullary thyroid carcinoma | 1 | |
| Anaplastic thyroid carcinoma | 1 |
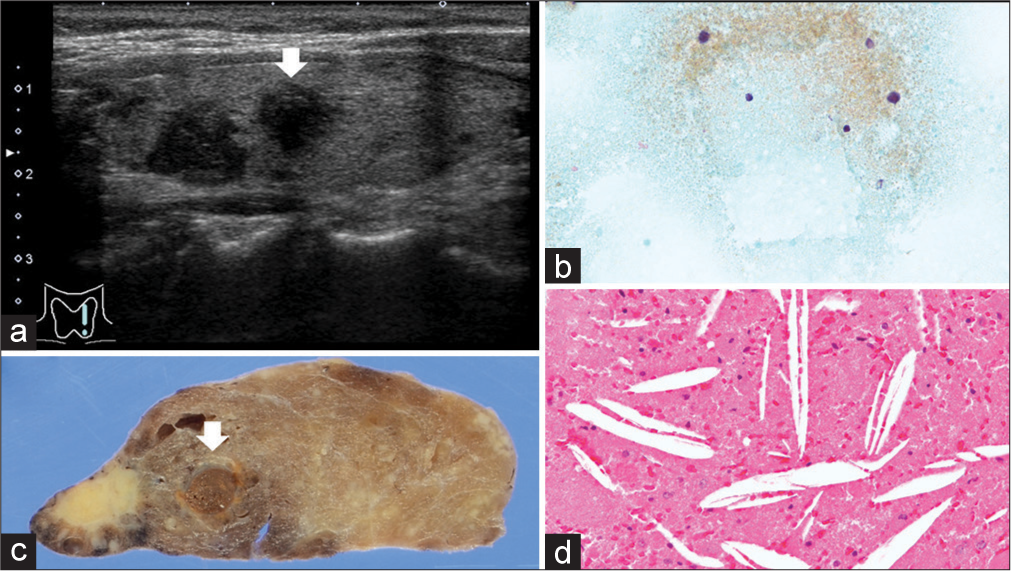
- Cystic follicular nodular disease. (a) Papillary thyroid carcinoma-suspected hypoechoic mass (white arrow) (Ultrasound B mode). (b) Cholesterol crystal and proteinaceous materials (Papanicolaou stain, x400). (c) Unilocular cystic lesion (white arrow). (d) Cholesterol crystal and proteinaceous materials (Hematoxylin and Eosin stain, x200).
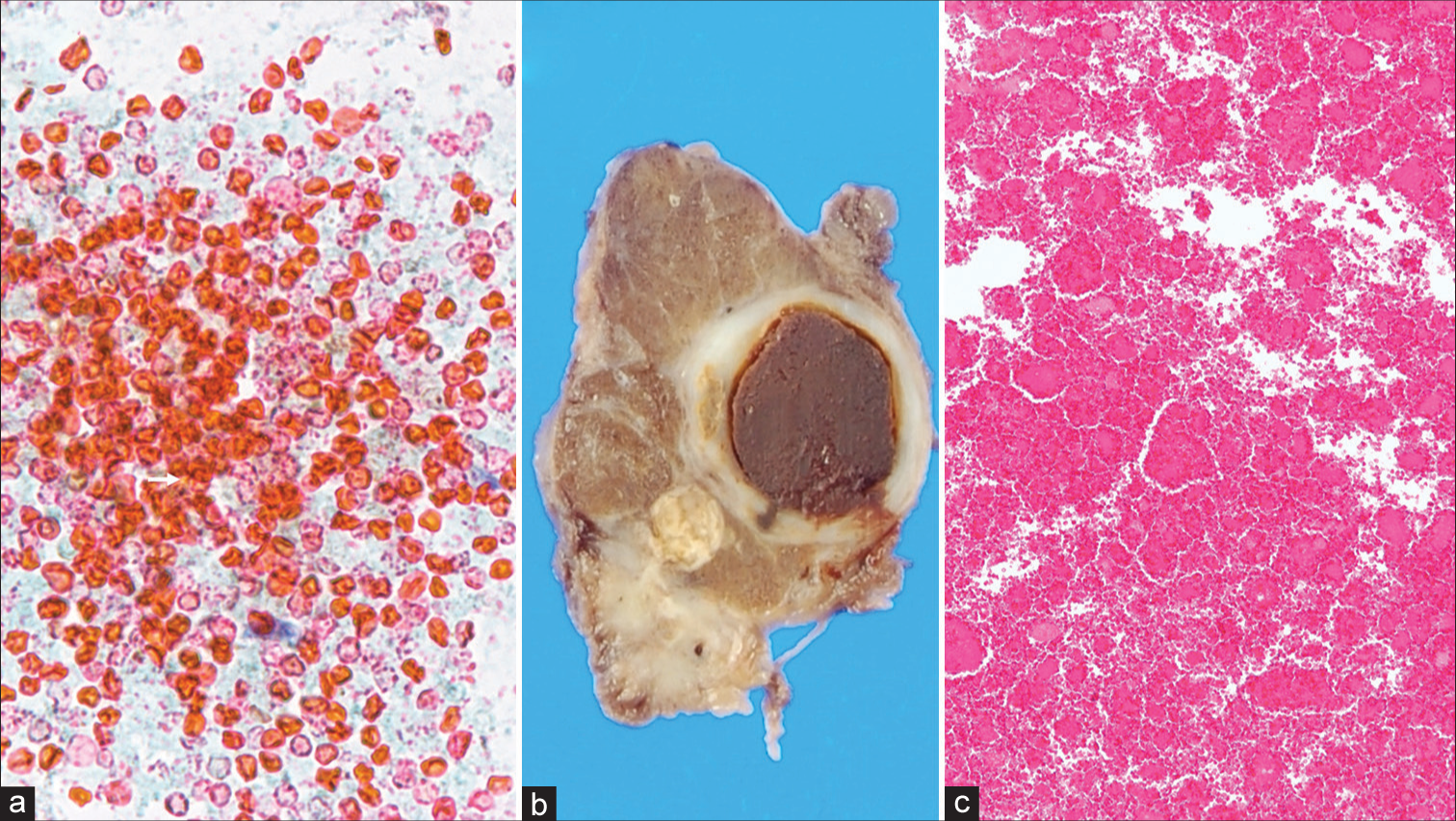
- Hemorrhagic follicular nodular disease. (a) Degenerative red blood cells (Papanicolaou stain, x400). (b) Cystic nodule containing blood clot. (c) Red blood cells (Hematoxylin and Eosin stain, x100).
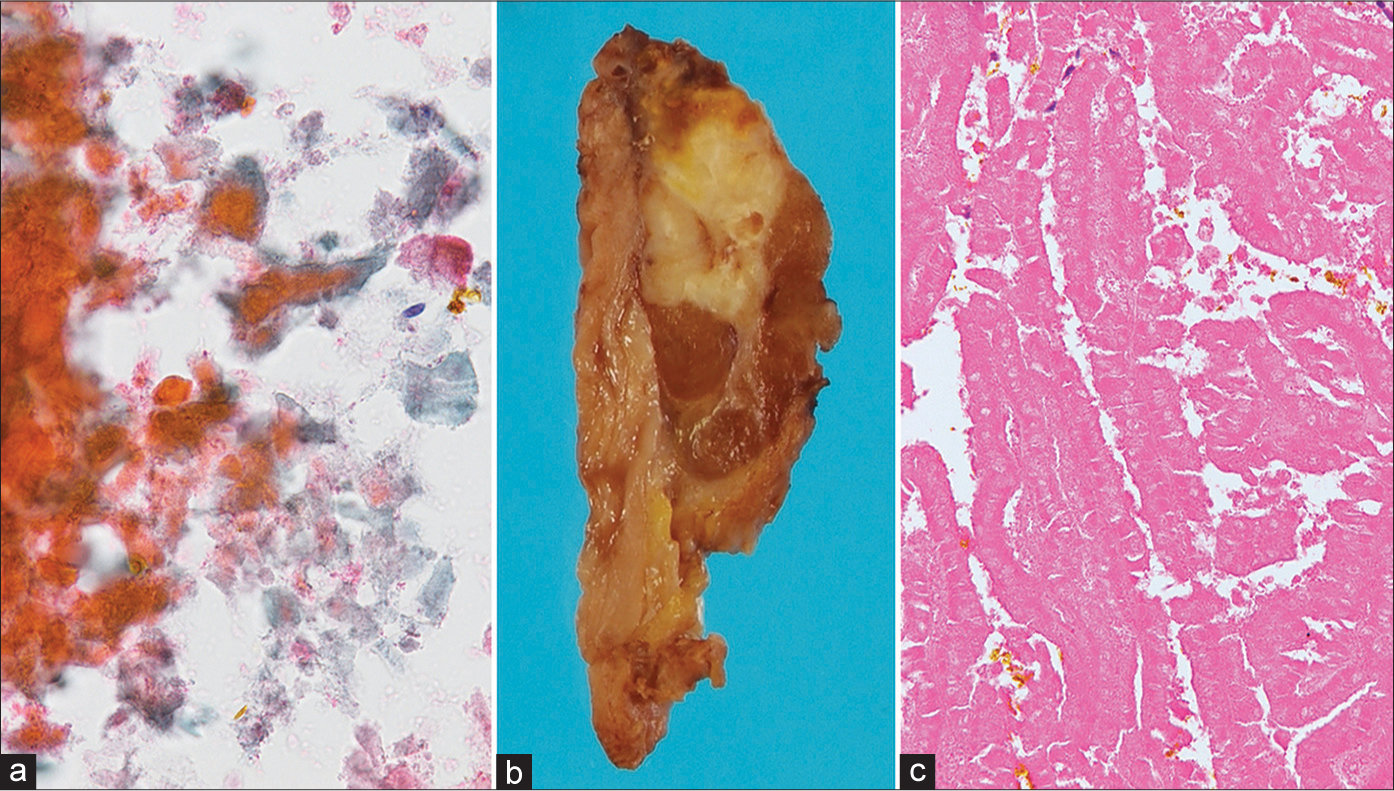
- Infarcted papillary thyroid carcinoma. (a) Necrotic cells (Papanicolaou stain, x400). (b) Solid tumor with focal necrotic area. (c) Coagulative necrosis of papillary thyroid carcinoma with papillary growth pattern. (Hematoxylin and Eosin stain, x200).
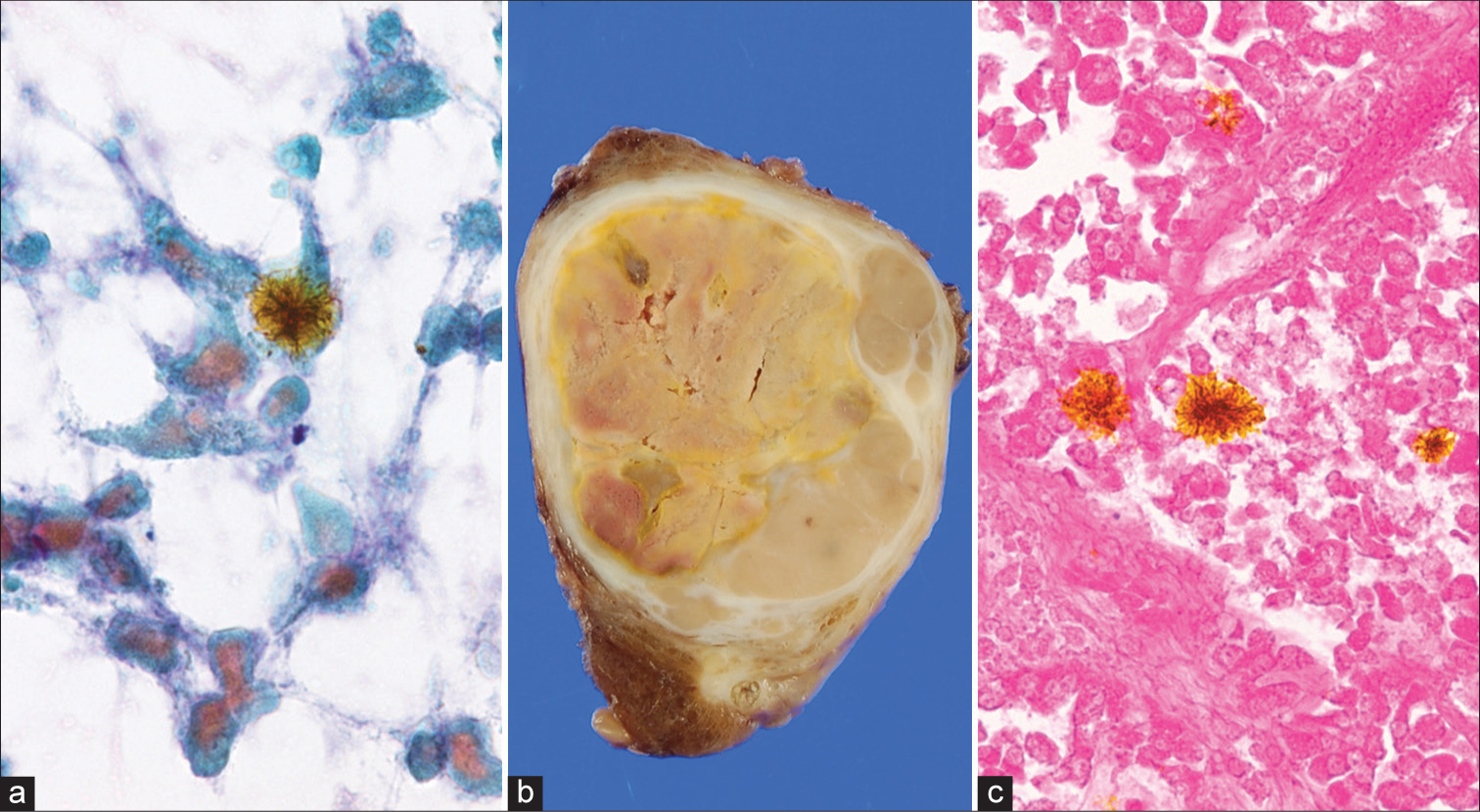
- Infarcted follicular thyroid carcinoma. (a) Necrotic cells and hematoidin (Papanicolaou stain, x400). (b) Encapsulated solid tumor with capsular invasio n and necrosis. (c) Necrotic carcinoma cells and hematoidin (Hematoxylin and Eosin stain, x200).
Resection rates and risks of malignancy
Table 5 shows the resection rates and risks of malignancy. The overall resection rate and risk of malignancy were 9.3% and 3.9%, respectively. The resection rates for nodules of malignancy suspected by ultrasound or FNA were 43.8% and 57.1%, respectively. The risk of malignancy for nodules categorized as cyst fluid and benign was 0%. The risks of malignancy for nodules interpreted as intermediate and high suspicion by ultrasound examination were 8.7% and 37.5%, respectively. The risk of malignancies for undetermined significance and malignancy nodules on FNAC were 37.5% and 57.1%, respectively. None of the patients with clay-like materials died during the follow-up.
| Ultrasound | Cytology | ||||
|---|---|---|---|---|---|
| Category | Resection rate | ROM (overall/resection) |
Category | Resection rate | ROM (overall/resection) |
| Non-classified (15) | 26.7% (4) | 13.3/50.0% (2) | Cyst fluid (124) | 4.0% (5) | 0/0% (0) |
| Benign (4) | 0% (0) | Benign (198) | 6.6% (13) | 0/0% (0) | |
| Very low suspicion (168) | 6.0% (10) | 1.2/20.0% (2) | Undetermined significance (16) | 43.8% (7) | 37.5/85.7% (6) |
| Low suspicion (129) | 7.0% (9) | 1.6/22.2% (2) | Follicular neoplasm (3) | 0% (0) | |
| Intermediate suspicion (23) | 13.0% (3) | 8.7/66.7% (2) | Suspicious for malignancy (0) | 0% (0) | |
| High suspicion (16) | 43.8% (7) | 37.5/85.7% (6) | Malignant (14) | 57.1% (8) | 57.1/100% (8) |
ROM: Risk of malignancy.
DISCUSSION
Implementation of rapid on-site evaluation reduced the non-diagnostic rate and improved the overall adequacy,[3,4,27,28] but the method is not widely available . On-site gross visual assessment is simple, fast, free of charge, and feasible for all patients, and can predict the adequacy of the samples.[7,10,11] Meena et al. prospectively demonstrated that the presence of defined as gooey white material on FNA aspirates correlated strongly with adequacy.[8] Granular materials on the preparation are likely to be diagnostic.[10,11] Williams et al. graded the macroscopic sample appearances on a five-point scale from 1 (blood with no particulate material) to 5 (solid tissue pieces); the positivity rate increased stepwise from 50% to 100% from grade 1 to grade 5 samples.[12] Neither granular materials nor solid tissue pieces have been observed in clay-like materials in the present study. However, cytological assessment of the clay-like materials was adequate in all nodules. Our study confirmed that clay-like materials are equivalent to grade 5, although they lacked solid tissue pieces. Therefore, the recognition contributes to avoiding unnecessary second punctures.
In the present study, most nodules with clay-like materials were cyst fluid or benign in FNA. These materials are mainly composed of non-epithelial components, including colloid or proteinaceous materials, foamy histiocytes, and degenerative red blood cells. Thus, the clay-like materials are likely derived from the contents of blood clots from benign cystic lesions. Similarly, Ren et al. described that hemorrhage appears as a reddish toothpaste-like muddy material in the early stage and brown bread-like material in the second stage of hemorrhage regression.[20] However, although rare, papillary thyroid carcinoma, follicular thyroid carcinoma, and medullary thyroid carcinoma aspiration materials can also contain clay-like materials. Moreover, the first two are observed when an infarction has occurred, and the latter when it contains abundant amyloid. The properties of clay-like materials must differ for benign and malignant lesions. If they were grossly subclassified based on their gross characteristics, our report would have been more worthwhile. However, it was not possible to subclassify them due to the retrospective nature of the study.
The American Thyroid Association management guidelines present the risk of malignancy according to each sonographic pattern. According to the guidelines,[22] the estimated risks of malignancy of high suspicion, intermediate suspicion, low suspicion, very low suspicion, and benign were 70–90%, 10–20%, 5–10%, <3%, and <1%, respectively. In comparison, the risk of malignancy (37.5%) of high suspicion in nodules with clay-like materials was considerably lower. We found that nodules with clay-like materials tended to be overestimated on ultrasonography. Concerning FNA, the risk of malignancy (37.5%) for undetermined significance in nodules with clay-like materials was considerably higher (16%) than that described in the Bethesda System,[29] whereas for malignancy, it was lower (57.1 vs. 94%). These findings demonstrate that FNA tends to be underestimated for thyroid nodules with clay-like materials.
SUMMARY
We investigated the diagnostic significance of clay-like materials aspirated from thyroid nodules. As the materials were considered sufficient specimens, the recognition contributes to avoiding unnecessary second punctures. Most of these are derived from the contents or blood clots of benign cystic lesions. The risk of malignancy was 3.9%, and the tumor could be a necrotic carcinoma due to infarction. Ultrasound examination tended to overestimate nodules with clay-like materials, whereas FNAC diagnosis tended to be more conservative. We should reaffirm that on-site gross visual assessment is a fast and reasonably accurate predictor of on-site adequacy of samples.
AVAILABILITY OF DATA AND MATERIALS
The data that support the findings of this study are available from the corresponding author, [RK], upon reasonable request.
ABBREVIATIONS
FNA: Fine-needle aspiration.
FNAC: Fine-needle aspiration cytology.
AUTHOR CONTRIBUTIONS
RK, MHir and AM: Designed the research study, performed the research; AS MHig, and TA: Provided help and advice on the experiments and analyzed the data; AM and TA: Critical revision of the article. All authors contributed to editorial changes in the manuscript. All authors have participated sufficiently in the work and agreed to be accountable for all aspects of the work. All authors read and approved the final manuscript.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was approved by the Ethics Committee of Kuma Hospital (approval no. 20200709-1). Written informed consent was obtained from all the par ticipants.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
EDITORIAL/PEER REVIEW
To ensure the integrity and highest quality of CytoJournal publications, the review process of this manuscript was conducted under a double-blind model (authors are blinded for reviewers and vice versa) through an automatic online system.
FUNDING
Not applicable.
References
- Fine-needle aspiration biopsy of thyroid nodules: Is routine ultrasound-guidance necessary? Surgery. 2018;164:789-94.
- [CrossRef] [PubMed] [Google Scholar]
- Standard needle magnetization for ultrasound needle guidance: first clinical experiences in fine-needle aspiration cytology of thyroid nodules. J Ultrasound Med. 2019;38:3311-9.
- [CrossRef] [PubMed] [Google Scholar]
- A new cytology staining method: A fast approach for rapid on-site evaluation on thyroid fine-needle aspiration cytology. Acta Cytol. 2023;67:289-94.
- [CrossRef] [PubMed] [Google Scholar]
- Rapid on-site evaluation with telecytology significantly reduced unsatisfactory rates of thyroid fine-needle aspiration. Am J Clin Pathol. 2020;153:342-5.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of diagnostic values of thyroid aspiration samples using liquid-based preparation and conventional smear: one-year experience in a single institution. APMIS. 2013;121:139-45.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of conventional smear and liquid-based cytology in adequacy of thyroid fine-needle aspiration biopsies without an accompanying cytopathologist. Sisli Etfal Hastan Tip Bul. 2022;56:353-9.
- [Google Scholar]
- The value of gross visual assessment of specimen adequacy for liquid-based cytology during ultrasound-guided, fine-needle aspiration of thyroid nodules. Endocr Pract. 2015;21:1219-26.
- [CrossRef] [PubMed] [Google Scholar]
- The Association of “GOOP” on Gross Examination of Fine Needle Aspiration Samples and On-Site Adequacy. Respiration. 2022;101:63-6.
- [CrossRef] [PubMed] [Google Scholar]
- Accuracy of visual on-site evaluation (Vose) In predicting the adequacy of Eus-guided fine needle biopsy: A single center prospective study. Pancreatology. 2021;21:312-7.
- [CrossRef] [PubMed] [Google Scholar]
- The utility of assessing the gross appearances of FNA specimens. Cytopathology. 2010;21:395-7.
- [CrossRef] [PubMed] [Google Scholar]
- The gross appearances of fine needle aspiration cytology samples. J Clin Pathol. 2009;62:57-9.
- [CrossRef] [PubMed] [Google Scholar]
- Macroscopic assessment of pulmonary fine needle aspiration biopsies: correlation with cytological diagnostic yield. Br J Radiol. 2002;75:28-30.
- [CrossRef] [PubMed] [Google Scholar]
- Prediction of nondiagnostic results in fine-needle aspiration of thyroid nodules: Utility of on-site gross visual assessment of specimens for liquid-based cytology. Endocr Pract. 2018;24:867-74.
- [CrossRef] [PubMed] [Google Scholar]
- Cytotechnologists and on-site evaluation of adequacy. Korean J Pathol. 2013;47:405-10.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnostic Clues for Thyroid Aspiration Cytology In: Kakudo K, ed. Thyroid FNA cytology differential diagnoses and pitfalls (2nd ed). Singapore: Springer; 2019. p. :1-18.
- [CrossRef] [Google Scholar]
- Unusual cytomorphology of acute suppurative thyroiditis. J Cytol. 2015;32:25-7.
- [CrossRef] [PubMed] [Google Scholar]
- Anaplastic thyroid carcinoma mimicking thyroid abscess. AME Case Rep. 2018;2:20.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnostic des kystes parathyroïdiens: intérêt du dosage de la parathormone dans le liquide de ponction [Diagnosis of parathyroid cysts: value of parathyroid hormone level in puncture fluid] Presse Med. 2000;29:939-41.
- [Google Scholar]
- Improvement in the detection of cystic metastatic papillary thyroid carcinoma by measurement of thyroglobulin in aspirated fluid. Biomed Res Int. 2016;2016:8905916.
- [CrossRef] [PubMed] [Google Scholar]
- Degenerating thyroid nodules: Ultrasound diagnosis, clinical significance, and management. Korean J Radiol. 2019;20:947-55.
- [CrossRef] [PubMed] [Google Scholar]
- Thyroid fine-needle aspiration and smearing techniques. VideoEndocrinology. 2018;5:ve.2018.0119.
- [CrossRef] [PubMed] [Google Scholar]
- 2015 American thyroid association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: The american thyroid association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid. 2016;26:1-133.
- [CrossRef] [PubMed] [Google Scholar]
- The Japanese reporting system for thyroid aspiration cytology 2019 (JRSTAC2019) Gland Surg. 2020;9:1653-62.
- [CrossRef] [PubMed] [Google Scholar]
- Thyroid FNA cytology: The eastern versus western perspectives. Cancer Cytopathol. 2023;131:415-20.
- [CrossRef] [PubMed] [Google Scholar]
- Introduction of histological classification and cytology reporting format of the Japanese General Rules for the Description of Thyroid Cancer with a special focus on the differences of the WHO Histological Classification and The Bethesda System of Thyroid Cytology. Endocr J. 2021;68:621-30.
- [CrossRef] [PubMed] [Google Scholar]
- Pathological diagnosis of general rules for the description of thyroid cancer by Japanese Society of Thyroid Pathology and Japan Association of Endocrine Surgery. Endocr J. 2022;69:139-54.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of rapid on-site evaluation on diagnostic accuracy of thyroid fine-needle aspiration. Acta Cytol. 2022;66:371-8.
- [CrossRef] [PubMed] [Google Scholar]
- The impact of rapid on-site evaluation on the quality and diagnostic value of thyroid nodule fine-needle aspirations. Thyroid. 2022;32:667-74.
- [CrossRef] [PubMed] [Google Scholar]
- The bethesda system for reporting thyroid cytopathology: Definitions, criteria, and explanatory notes. (3rd ed). New York: Springer; 2023.
- [CrossRef] [Google Scholar]









