Translate this page into:
Parakeratotic-like cells in effusions — A clue to diagnosis of malignant mesothelioma
*Corresponding author
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Malignant mesothelioma (MM) is an aggressive neoplasm with a poor prognosis. Its incidence has been increasing worldwide. Cytological examination of an effusion is often the first opportunity to diagnose MM. However, the cytological diagnosis of MM can be difficult. We have noticed that parakeratotic-like cells, with orange cytoplasm and pyknotic nuclei, are present in many cases of mesothelioma on Papanicolaou-stained cytology slides. Although this cytological finding has been described previously, to our knowledge, there has been no systematic study of this finding. Our study is to determine whether the presence of small parakeratotic / orangeophilic cells (PK-like cells) is specific for the cytodiagnosis of mesothelioma.
Materials and Methods:
A total of 90 body fluid cases were selected from our archived specimens in the Cytology Section at the University of Chicago Hospital accessioned between January 2000 to November 2011. They included 30 cases of mesothelioma, 30 cases of adenocarcinoma, and 30 cases of reactive mesothelial cells.
Results:
PK-like cells were present in 83% of the mesothelioma cases, 13% of the adenocarcinoma cases, and 7% of the reactive cases. Our data showed that the presence of PK-like cells has a specificity of 90%, sensitivity of 83%, positive predictive value of 81%, and negative predictive value of 84% for the diagnosis of malignant mesothelioma in body cavity fluids.
Conclusion:
The presence of PK-like cells in the effusion specimen, especially in pleural effusions, is a highly specific and moderately sensitive cytological feature for diagnosis of mesothelioma.
Keywords
Adenocarcinoma
effusion
malignant mesothelioma
parakeratotic-like cells
INTRODUCTION
Malignant mesothelioma (MM) is an aggressive neoplasm with a poor prognosis. Approximately 3300 new cases of MM are diagnosed annually in the United States,[1] and about 85% of the MM are present with pleural disease, although MM can also arise in other locations, including the peritoneum, pericardium or tunica vaginalis.[2] The major risk factor is asbestos exposure; however, other factors such as the Simian virus 40 infection and inheritance of susceptibility genes are likely to play a role.[34] Although MM has a limited response to surgery, conventional chemotherapy, and radiotherapy,[1] recent clinical trials have suggested that the combination of pemetrexed plus cisplatin improve survival and quality of life[56] in MM patients. Therefore, early diagnosis of MM is important, because it may significantly improve a patient's survival.[7] As the disease manifests initially as a recurrent, unilateral, bloody pleural effusions in most patients,[8] the cytological examination of the effusion fluid can provide a simple and fast diagnostic test. However, the reported sensitivity and specificity for the cytological diagnosis of MM varies greatly in literature,[9] due to the lack of specific cytological features of MM. We have noticed that many mesothelioma cases have parakeratotic-like small, orange cells with pyknotic nuclei (PK-like cells)[10] on Papanicolaou-stained cytology slides. This feature was previously described by Whitaker[11] as an uncommon, but fairly specific feature of MM. However, to our knowledge, there is no systematic study of this finding for the diagnosis of MM. Our study was aimed at determining the sensitivity and specificity of the presence of PK-like cells for the diagnosis of mesothelioma.
MATERIALS AND METHODS
Thirty cases of histologically documented malignant mesothelioma, with corresponding body cavity fluid cytological specimens (pleural effusions, ascites, pericardial effusions) were selected from the archived material in the Cytology Section of the University of Chicago Hospital, accessioned between January 2000 and November 2011. All cases were epithelioid type of MM, confirmed by histological and immunological studies. Control groups included 30 cases with a diagnosis of reactive mesothelial cells and 30 cases of adenocarcinoma in body fluids. The body fluids were spun down and were then processed with standard Cytospin and ThinPrep protocols. Only slides stained with the Papanicolaou method were selected for this study. There was no difference noticed on the slides with regard to the color or cytology by both Cytospin and ThinPrep protocols.
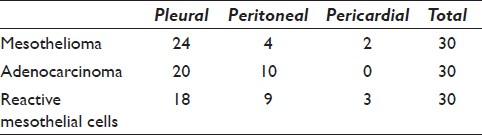
Of the 30 MM cases, 24 cases were from pleural effusions, four cases were from ascites, and two were from pericardial effusions. Of the 30 adenocarcinoma cases, 20 cases were from pleural effusions and ten cases were from ascites. In the adenocarcinoma group, nine cases had previous histological diagnosis of breast adenocarcinoma, seven cases had previous histological diagnosis of papillary serous adenocarcinoma, ovarian or fallopian tube primary, and five cases were diagnosed histologically with pancreatic adenocarcinoma; the other diagnoses included endometrioid, lung, thyroid and renal cell carcinoma. Of the 30 reactive cases, 18 cases were from pleural effusions, nine cases from ascites, and three cases from pericardial effusions [Table 1].
All 90 cases were previewed for parakeratotic-like cells by the cytology Fellow (LG), two slides of each case and the one with more PK-like cells was chosen for review and confirmation by two board-certified cytopathologists (WR, RMD). Parakeratotic-like cells were defined as small, degenerated cells, with orangeophilic cytoplasm and degenerated, pyknotic nuclei. Any case that had PK-like cells was counted as positive. Cases with cells that had orange cytoplasm, but were without degenerated pyknotic nuclei, were counted as negative. Similarly, cases that had cells with eosinophilic cytoplasm were counted as negative regardless of the nuclear structure. These eosinophilic cells often had a blue staining ectoplasmic rim, whereas, the PK-like cells were orange throughout the cytoplasm.
Statistical analysis
The sensitivity, specificity, positive and negative predictive values of cases with PK-like cells for the diagnosis of mesothelioma were calculated as follows:
Sensitivity = True positive / (True positive + False negative)
Specificity = True negative / (True negative + False positive)
Positive predictive value = True positive /(True positive + False positive)
Negative predictive value = True negative /(True negative + False negative)
RESULTS
The two key features of PK-like cells were: pyknotic nuclei and orange cytoplasm [Figure 1]. The PK-like cells were usually smaller than the mesothelial cells, whether benign or malignant. Some mimics were identified, which showed only orange cytoplasm without pyknotic nuclei or eosinophilic (pink) cytoplasm, with or without pyknotic nuclei: these were not counted as PK-like cells [Figure 2].
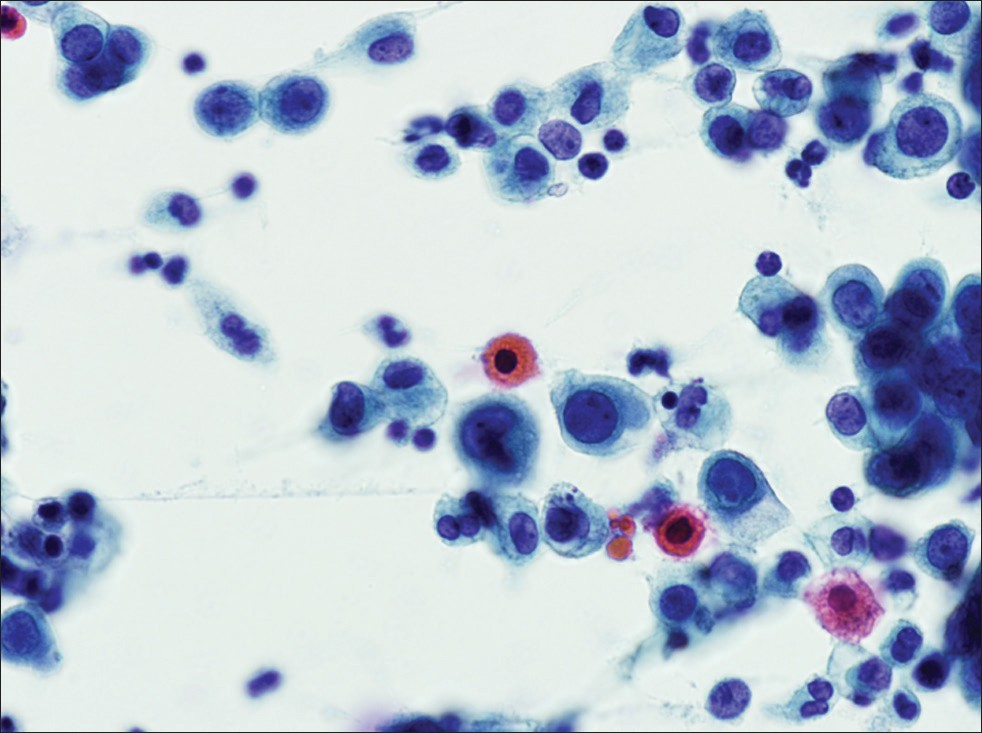
- Parakeratotic-like cell. Parakeratotic-like cells are small, degenerated orangeophilic cells with pyknotic nuclei that look like parakeratotic cells in the Pap test (Pap stain, ×400)
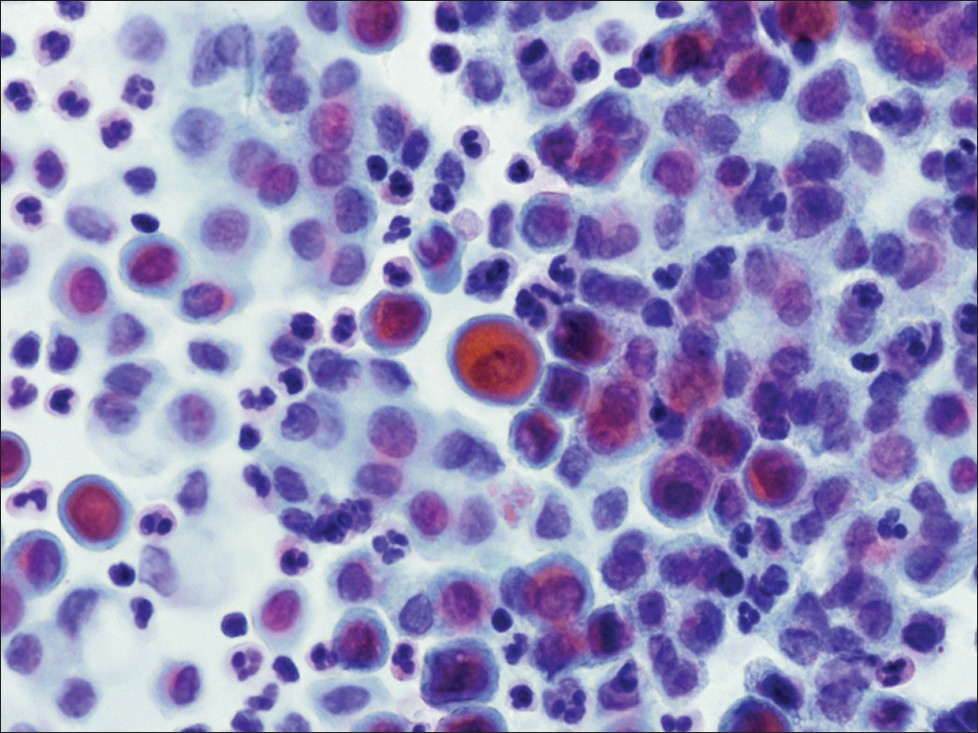
- Mimickers of PK-like cells. Cells that had orangeophilic cytoplasm, but lacked degenerated pyknotic nuclei or cells with eosinophilic cytoplasm (regardless of nuclear structure) were not counted as PK-like cells. These mimicker cells typically had a rim of blue staining cytoplasm (Pap stain, ×400)
Table 2 shows the summary of mesothelioma cases with various PK-like cells. Seven of the 30 cases showed numerous (> 5 / slide) PK-like cells, but these were usually less than 1% of the total cell population. Eight cases showed moderate (3 – 5 / slide) PK-like cells that were easily identified. Ten cases had only rare (1 – 2 / slide) PK-like cells. No PK-like cells were identified in five mesothelioma cases and these five cases were either poorly cellular or had papillary structures.

Four of the 30 adenocarcinoma cases (17%) had rare-(two cases)-to-moderate (two cases) PK-like cells [Table 3]. All four positive adenocarcinoma cases were ovarian serous papillary adenocarcinoma, which accounted for 57% (4 / 7) of the serous papillary adenocarcinomas.

The PK-like cells were present in 83% of the mesothelioma cases, 13% of the adenocarcinoma cases and 7% of the reactive cases. In non-mesothelioma cases, when PK-like cells were present, they were usually rare. Table 4 summarizes these findings.

In the present study, the sensitivity of PK-like cells for the diagnosis of mesothelioma was 83%, the specificity was 90%, the positive predictive value was 81%, and the negative predictive value was 84%. When moderate or many PK-like cells were present, the specificity was 97%, but the sensitivity dropped to 50%.
DISCUSSION
Our results showed that the presence of PK-like cells in effusion specimens was highly specific for the diagnosis of MM, especially when the PK-like cells were moderate or numerous. In reactive and adenocarcinoma cases, the PK-like cells were identified in only 7% (reactive) or 13% (adenocarcinoma) of cases, and when present, the PK-like cells were sparse. Interestingly, among adenocarcinomas, the PK-like cells were noted only in ovarian serious papillary adenocarcinoma (SPA) and not in other adenocarcinomas. The PK-like cells are present in four of seven (57%) SPA cases [Table 3]. Of the seven SPA cases, only one case was from a pleural effusion (the others were ascites), while 24 of the 30 mesothelioma cases were pleural effusions [Table 1].
Mesothelioma cases that were negative for PK-like cells were either poorly cellular or had papillary architecture. The total number of PK-like cells rarely exceeded about 1% of the total cellularity; therefore, the probability of identifying PK-like cells in a hypocellular specimen was correspondingly low. However, it was not obvious why PK-like cells were not present in those cases of MM with papillary architecture.
The formation of PK-like cells seems to be a degenerative change in the malignant mesothelial cells. The nuclei are pyknotic, indicating cell death, and the cytoplasm also appears granular and degenerated. We speculate that the PK-like cells may represent a form of apoptosis. Mesothelial cells not only contain keratins, but also when any cell type degenerates, they can stain with Orange G, the component of the Papanicolaou stain responsible for orangeophilia.[10] It is possible that chemicals, such as hyaluronic acid,[12] in the effusion play a role in the development of the PK-like cells in MM. Although squamous metaplasia in the mesothelioma has been described,[13] it seems less likely that squamous metaplastic cells are the small orange cells, based on their rarity and morphology.
Cytology plays an important role in the detection of mesothelioma. As patients often present with effusions, examination of the effusion fluid is often the first specimen submitted in the work-up of the mesothelioma. The cytodiagnosis of the mesothelioma can be challenging, because the malignant cells can closely resemble benign, reactive mesothelial cells. Failure to recognize the cells as malignant could lead to a delay in diagnosis if the patient is treated for a benign effusion. Therefore, a morphological clue to diagnosis that is often present in mesothelioma (sensitive) and usually absent in other diseases (specific), such as the PK-like cells described here, could be very helpful in the recognition of malignant mesothelioma. However, the Papanicolaou stain can vary among laboratories, so it is possible that our results are not entirely representative. Therefore, the relation between PK-like cells and MM may need further study in different laboratories, to confirm its usefulness.
In conclusion, our study showed that the presence of PK cells in pleural effusion is a highly specific and moderately sensitive cytological feature for the diagnosis of mesothelioma in the effusion specimens. The major differential diagnosis is serous papillary carcinoma.
COMPETING INTEREST STATEMENT BY ALL AUTHORS
The authors declare that they have no competing interests.
AUTHORSHIP STATEMENT BY ALL AUTHORS
All authors of this article declare that they qualify for authorship as defined by the ICMJE http://www.icmje.org/#author. Each author has participated sufficiently in the study and take public responsibility for the appropriate portions of the content of this article. Each author acknowledges that this final version was read and approved.
ETHICS STATEMENT BY ALL AUTHORS
This study was conducted with approval from the Institutional Review Board.
EDITORIAL / PEER-REVIEW STATEMENT
To ensure the integrity and highest quality of CytoJournal publications, the review process of this manuscript was conducted under a double blind model (authors are blinded for reviewers and vice versa) through automatic online system.
Available FREE in open access from: http://www.cytojournal.com/text.asp?2012/9/1/18/99170
REFERENCES
- Update on malignant pleural mesothelioma. Semin Respir Crit Care Med. 2011;32:102-10.
- [Google Scholar]
- Early stages of mesothelioma, screening and biomarkers. Recent Results Cancer Res. 2011;189:169-93.
- [Google Scholar]
- Mesothelioma epidemiology, carcinogenesis, and pathogenesis. Curr Treat Options Oncol. 2008;9:147-57.
- [Google Scholar]
- Simian virus 40 transformation, malignant mesothelioma and brain tumors. Expert Rev Respir Med. 2011;5:683-97.
- [Google Scholar]
- Chemotherapy and targeted therapies for unresectable malignant mesothelioma. Lung Cancer. 2011;73:256-63.
- [Google Scholar]
- Systemic treatments for mesothelioma: standard and novel. Curr Treat Options Oncol. 2008;9:171-9.
- [Google Scholar]
- Current status of screening for malignant pleural mesothelioma. Semin Thorac Cardiovasc Surg. 2009;21:97-104.
- [Google Scholar]
- The sensitivity of cytologic evaluation of pleural fluid in the diagnosis of malignant mesothelioma. Diagn Cytopathol. 2010;38:874-9.
- [Google Scholar]
- The Art and Science of Cytopathology. (2nd ed). Chicago: ASCP Press; 2012. p. :319.
- [Google Scholar]
- Cytological diagnosis of malignant mesothelioma--improvement by additional analysis of hyaluronic acid in pleural effusions. Virchows Arch. 2007;450:455-61.
- [Google Scholar]
- Malignant peritoneal mesothelioma with squamous metaplasia. Cytopathology. 1993;4:373-8.
- [Google Scholar]








