Translate this page into:
Cytologic smears improve accuracy of frozen sections of ovarian tumors in the community practice settings
*Corresponding author
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
The ovaries can be the site for various primary tumors and also the presenting site of metastatic disease. Quick and correct intraoperative diagnosis is crucial for the patient's further management. The aim of this study was to demonstrate the advantages of the combined diagnostic method – ovarian frozen sections in conjunction with cytologic smears.
Methods:
From June 2016 to June 2017, we prospectively prepared additional two cytologic smears with Diff-Quik stain on ovarian frozen sections comprised of two hematoxylin and eosin sections. For quality assurance purposes, we compared the results of frozen section discrepancies and deferrals with those that of the previous year from June 2015 to June 2016.
Results:
With the introduction of cytologic smears to ovarian frozen sections, the number of discrepancies and deferrals combined decreased from 13.75% to 7.85%. The most benefit of smears was observed in primary ovarian malignancies.
Conclusions:
In the setting where all the members of the pathology group render cytologic evaluations routinely, smears play an important complementary role.
Keywords
Cytology smears
ovarian frozen section
ovarian tumors
touch imprint cytology
INTRODUCTION
The ovaries can be the site for various pathologies, from benign to malignant with the added problem of borderline lesions, and can also be the presenting site of metastatic disease. Quick and correct intraoperative diagnosis of ovarian lesions offers a possibility of adequate one-stage surgery, reducing the need for a second surgery with its inherent risks and helps to plan further management.[1] This approach benefits all patients, especially when fertility needs to be preserved.
Frozen section is the main diagnostic procedure used for the intraoperative assessment of ovarian lesions with an overall accuracy of 86%–97%.[2] However, this diagnostic tool has its own limitations, usually related to the sampling errors or technical problems, such as freezing artifacts.[123] During the past decade, the application of both cytological smears and frozen sections for intraoperative diagnosis of ovarian pathology has been discussed. Most of the studies compare these two methods and their efficacy and accuracy. Cytological smears have been shown as an easy to perform and inexpensive technique which can preserve cellular details.[4] Cytological evaluation is also superior to frozen sections in the diagnosis of select types of ovarian neoplasms,[5] but in general frozen section diagnosis is reported to be more accurate and sensitive than that of cytological smears alone, and the latter should play mostly a very useful complementary role.[16789]
Only a few studies investigate the value of combining intraoperative diagnostic use of both cytology and frozen sections.[101112] The aim of this study is to demonstrate the advantages in the application of a combined method. This study proved that the combined method leads to a decrease in a number of deferrals and discrepancies with the final histological diagnosis in comparison with the use of frozen sections method alone.
METHODS
At our institution, which is a 711-bed tertiary care medical center and cancer center, we perform on average 1031 frozen sections per year, of which 18% are related to gynecologic pathology. All pathologists who perform frozen sections routinely sign out general both surgical pathology and cytopathology.
From June 2016 to June 2017, we prospectively prepared additional cytologic imprints with Diff-Quik stain on ovarian frozen sections. Two cytologic imprints were taken from different areas of the tumor in addition to one standard section for frozen section. Two sections from different areas were obtained for mucinous tumors. For quality assurance purposes, we compared the results of frozen section discrepancies and deferrals with those that of the previous year from June 2015 to June 2016.
We used very strict criteria for deferrals and discrepancies and, therefore, the number of deferrals and discrepancies appear quite large. Every tumor that was not further subclassified (for example adenocarcinoma without characterizing it as high-grade or favor primary cancer) was considered discrepant for purposes of this study. The criteria were established based on a need in a high-volume cancer center to better identify the high-grade primary ovarian carcinomas that may require chemotherapy and placement of a catheter to administer the chemotherapy at the time of the initial surgery.
During the period from June 2015 to June 2016, we performed 164 intraoperative gynecologic consultations, including 80 ovarian frozen sections that were selected for this study and formed Group 1 [Table 1]. From June 2016 to June 2017, 167 intraoperative gynecologic consultations were done including 76 ovarian frozen sections that formed Group 2 [Table 1].
| Year | 2015/2016 (Group 1) | 2016/2017 (Group 2) |
|---|---|---|
| Total number of frozen sections | 780 | 1282 |
| Gynecologic intraoperative consultations | 164 | 167 |
| Ovarian frozen sections | 80 | 76 |
| Primary high-grade carcinoma deferred/discrepant | 4 | 1 |
| Granulosa cell tumor deferred/discrepant | 1 | 0 |
| Others (including borderline tumors, spindle cell tumors, and metastatic lesions) deferred/discrepant | 6 | 5 |
| Percentage of deferrals/discrepancies | 13.75 | 7.89 |
Group 1 comprised 57 benign, five borderlines, 17 malignant, and one other primary ovarian tumors (granulosa cell tumor). Group 2 comprised 45 benign cases, 11 borderline tumors, 16 malignant, and four other primary ovarian tumors (two granulosa cell tumors, a yolk sac tumor, and a sex cord stromal tumor with heterologous elements).
RESULTS
The total number of cases was comparable in both the groups, 80 cases in Group 1 and 76 cases in Group 2. The number of malignant cases was similar – 17 and 16, respectively.
Among the malignant cases in both groups, the diagnosis of serous carcinoma was prevalent – 12 out of 17 and 11 out of 16 malignancies, respectively. In the first group, 4 out of 12 serous carcinomas were diagnosed as adenocarcinoma without further sub-classification (such as high-grade or favor serous carcinoma). Adding the examination of the cytologic smears in Group 2 reduced this number to 1 out of 11 serous carcinomas without sub-classification. Clear cell carcinoma and particularly tubulocystic variant can be difficult to diagnose at the time of frozen section and this diagnosis was deferred in Group 1 [Table 2]. In Group 2, cytologic smears improved the accuracy for this malignant neoplasm leaving no deferred/discrepant cases for clear cell carcinomas. Besides the serous carcinomas and clear cell carcinoma, two more malignant diagnoses were deferred/discrepant in Group 1– a mucinous adenocarcinoma and carcinosarcoma.
| 2015/2016 (Group 1) | 2016/2017 (Group 2) | ||
|---|---|---|---|
| Frozen section diagnosis | Final diagnosis | Frozen section diagnosis | Final diagnosis |
| Adenocarcinoma, NOS (4 cases) | High-grade serous carcinoma | Adenocarcinoma NOS (1 case) | High-grade serous carcinoma |
| Benign cyst | Clear cell carcinoma | Extensive endometriosis | Adenosarcoma |
| Spindle cell lesion | Mesothelioma | Spindle cell lesion | Endometrial stromal sarcoma |
| Borderline mucinous lesion | Mucinous adenocarcinoma | Mucinous cystadenoma | Mucinous borderline tumor |
| Benign cyst | Granulosa cell tumor | Germ cell tumor | Sex cord stromal tumor with heterologous elements |
| Low-grade spindle cell lesion | Fibroma | Spindle cell lesion | Gastrointestinal stromal tumor |
| High-grade malignancy cannot rule out metastasis | Carcinosarcoma | ||
| Adenocarcinoma | Mesothelioma | ||
NOS: Not otherwise specified
Among the other types of ovarian tumors, a granulosa cell tumor in Group 1 was deferred, [Table 2] whereas in Group 2 two granulosa cell tumors were correctly diagnosed in conjunction with cytologic smears.
The cytologic examination was not helpful with borderline tumors [Table 2] with a discrepancy for each year. Furthermore, the cytologic examination was not particularly useful with rare and unusual spindle cell malignancies involving the ovary.
Overall, the diagnostic accuracy with cytologic examination improved, and the number of deferred and discrepant cases decreased from 13.25% to 7.89% demonstrating the benefit of adding cytologic smears.
DISCUSSIONS
Ovarian frozen sections are relatively common. Complex masses and enlarging cystic lesions, especially in postmenopausal patients are an indication for a frozen section. Establishing the frozen section diagnosis is important for further procedures at the time of surgery. Knowing the patient's age, clinical history, imaging studies, and serum markers are very helpful, but in the end, the diagnosis is made based on gross and microscopic findings.
During the intraoperative consultation for ovarian pathology, it is important to distinguish between primary adenocarcinoma versus metastatic carcinoma. In addition, the pathologist should at least favor high-grade versus low-grade carcinoma.
Usually, after reviewing gross findings, one or two sections can be sampled at the time of surgery. However, the advantage of cytologic sampling is that the imprint can be easily obtained from different parts of the tumor. Since also cytology does not require freezing, cutting, and staining of multiple slides, it can be performed very quickly. Moreover, often frozen section artifact hampers the evaluation of nuclear and cytologic details and having corresponding cytology preparation may give the pathologists a more complete appreciation of nuclear and cytologic features to and help in establishing the diagnosis.
The accuracy and importance of intraoperative cytologic preparations are well-documented in other organ systems, particularly in the central nervous system and breast sentinel lymph nodes.[1314]
In this study, we found cytologic smears very useful for high-grade primary carcinomas. Cytologic features of serous carcinoma are similar to histologic features with large nuclei with 3:1 ratio of adjacent cells, prominent nucleoli, frequent mitotic figures, papillae, and psammoma bodies. While these features can be appreciated on frozen section slide, they are much easier observed on cytologic imprints and smears. Furthermore, frozen section of more solid serous carcinoma is usually rather challenging [Figure 1a]. Smears usually highlight papillary structures, increased cellularity, and discohesive nature of the cells [Figure 1b]. Psammoma bodies can be also appreciated.
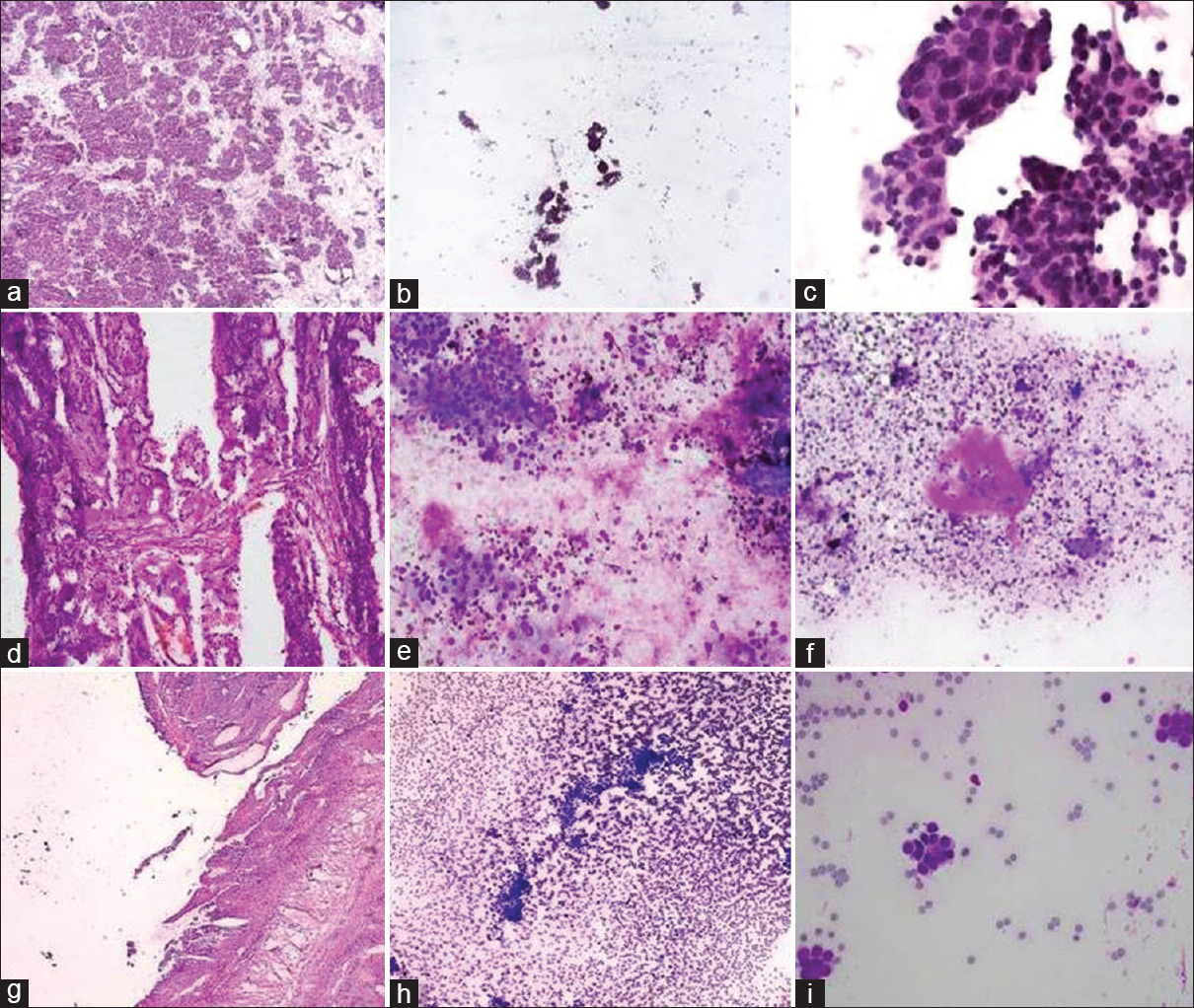
- (a) Solid serous carcinoma frozen section slide. (b and c) Papillary structures with high-grade cells cytology imprint. (d) Clear cell carcinoma frozen section slide. (e and f) High-grade cells with hyaline background. (g) Granulosa cell tumor frozen section slide. (h and i) Bland uniform nuclei and Call-Exner bodies’ cytology imprint
Clear cell carcinoma can be notoriously deceiving and difficult to diagnose on the frozen slide. If the tumor is mostly cystic or tubulocystic, it can be misdiagnosed resulting in the second surgery. Smears highlight high-grade cells sometimes with a hyaline background [Figure 1e and f]. In this study, we had two cases of clear cell carcinoma and the one with cytologic smear was correctly diagnosed at the time of frozen section.
Endometrioid tumors arising from endometriosis enter into the differential diagnosis of serous carcinoma. Endometrioid adenocarcinoma shows more cohesive groups of columnar cells and occasionally rare squamous morules with acute inflammation [Figure 2]. Squamous morules when identified easily establish the diagnosis, but are not always conveniently present [Figure 2c].
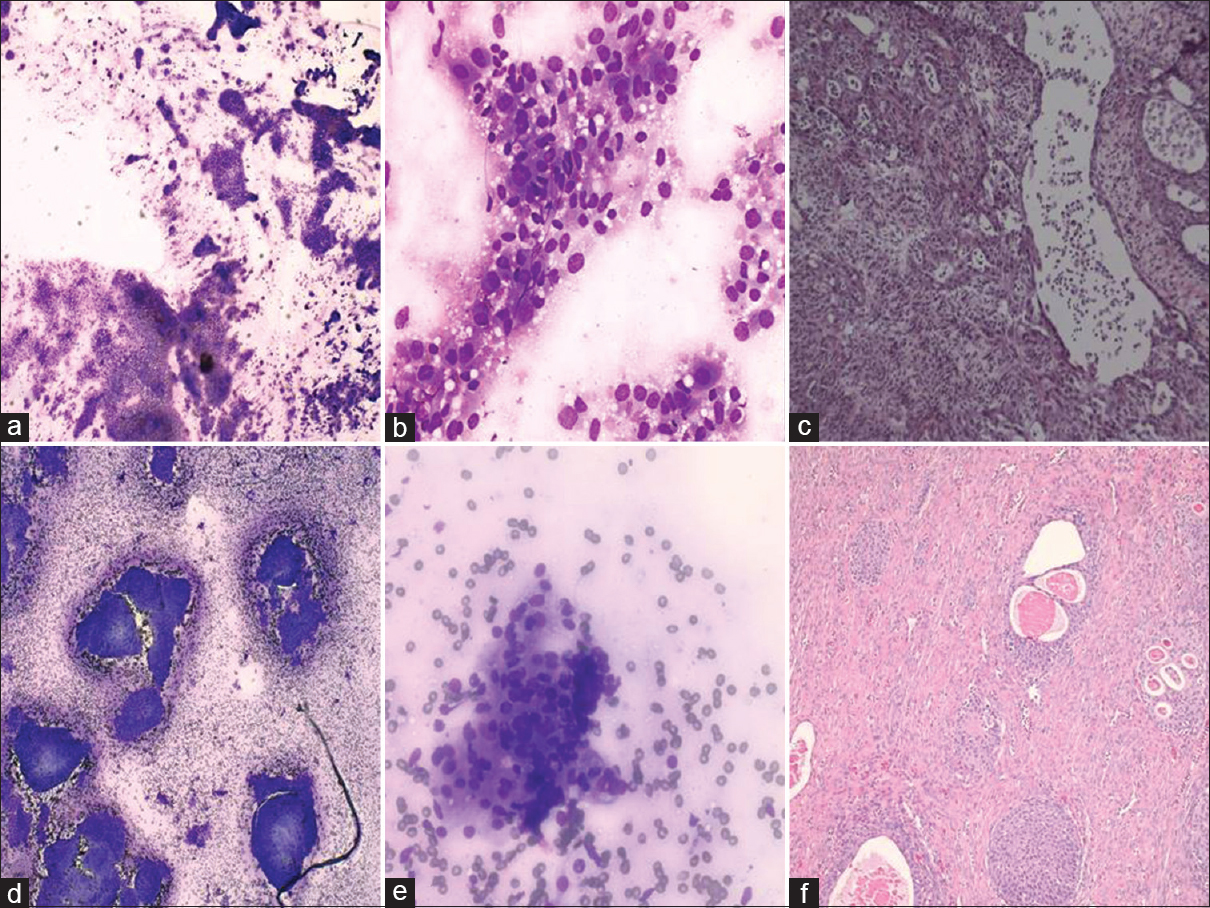
- (a and b) Endometrioid tumor of the ovary - cohesive groups of columnar cells. (c) Corresponding frozen section shows no squamous morules. (d) Brenner tumor - cellular smear of cohesive clusters. (e) High power shows uniform cells with low nuclear-cytoplasmic ratio (f) Corresponding permanent section of Brenner tumor
The other subset of tumors that can be deceiving and difficult at the time of frozen section is granulosa cell tumors. In addition to gross findings (variegated yellow-hemorrhagic cut surface), cytology smears are extremely helpful. Bland nuclear features with grooves can be easily appreciated on smears. It is also not unusual to see true Call–Exner bodies [Figure 1].
Benign lesions can be easily diagnosed on frozen sections. Both gross finding and microscopic findings are straightforward in the majority of the cases. The only exception on cytology smears is Brenner tumor. Brenner tumor can be cellular with uniform cells forming cohesive clusters [Figure 2d and e]. However, in conjunction with frozen section slide and gross findings, it should not be difficult to render the correct diagnosis [Figure 2f].
Metastatic lesions are important, although sometimes difficult to recognize during the time of frozen section. While there are soft criteria (bilateral, nodular tumors with size <13 cm, hilar involvement, extensive lymphovascular invasion, etc.) to help the pathologist suspect a metastatic lesion, many times primary tumors have similar features. Among most helpful cytologic features of metastatic malignancies are abundant mucin that correlates with dissecting mucin on histology, signet cell or fine “salt-and-pepper” chromatin and extensive necrosis with numerous neutrophils [Figure 3].
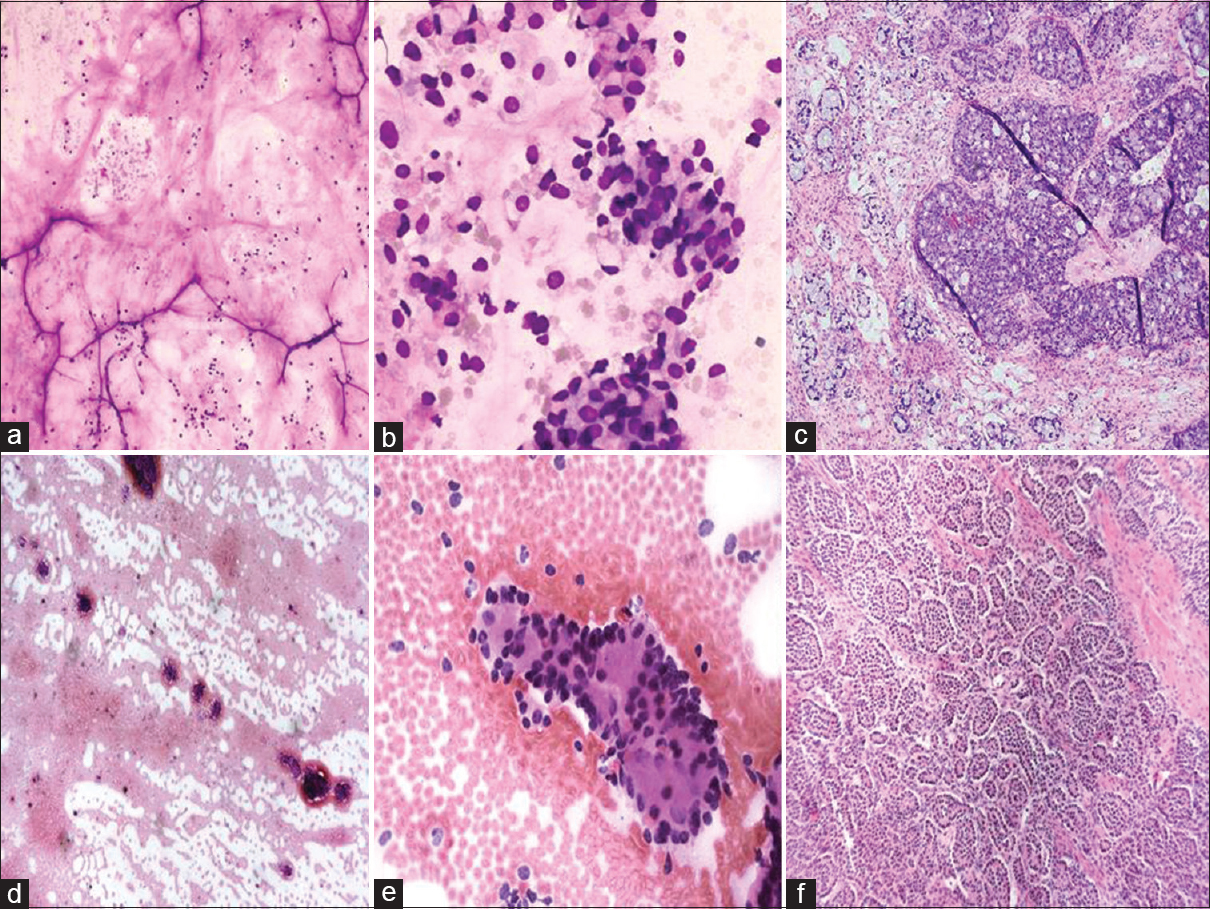
- (a and b) Abundant mucin and signet cells are unusual features for primary ovarian cancer. (c) Corresponding section shows metastatic adenocarcinoma arising from appendiceal primary. (d and e) The smears show moderately cellular smears with fine “salt-and-pepper” chromatin. (f) Corresponding section of metastatic neuroendocrine tumor
In our experience, smears were not extremely helpful for spindle cell lesions or borderline tumors. Spindle cell lesions of the ovary included in this study were somewhat unusual and rare. For example, at the time of frozen section, the smears did not contribute to the diagnosis of adenosarcoma or endometrioid stromal sarcoma [Table 2].
A retrospective study by Azami et al.[5] had similar results to this study where cytologic smears were extremely helpful for the diagnosis of malignancy. Two other retrospective studies by Alvarez Santín et al.[9] and Souka et al.[10] showed that cytology smears are important and helpful as a complementary method in the ovarian frozen sections. The study by Abe et al.[12] wonderfully described the significance of cytologic preparation for germ cell tumors at the time of surgery. In this study, we did not have many germ cell tumors to compare. Mature cystic teratomas were quite accurately diagnosed with or without cytologic smears. No immature teratomas were submitted for the intraoperative consultation in observed 2 years period. In the case of yolk sac tumor, the cytologic imprint was prepared but the significance of the imprint contribution remains uncertain since the pathologist was already aware of the extremely high levels of serum alpha-fetoprotein.
CONCLUSIONS
In community practice settings where all pathologists practice cytology, cytologic smears are valuable in improving accuracy and play an important complementary role in ovarian pathology at the time of frozen section.
COMPETING INTERESTS
The authors declare that they have no competing interests.
AUTHORSHIP STATEMENT BY ALL AUTHORS
All authors of this article declare that we qualify for authorship as defined by ICMJE http://www.icmje.org/#author.
Each author has participated sufficiently in the work and takes public responsibility for appropriate portions of the content of this article.
AC performed acquisition of data, its analysis and interpretation, and drafted the article.
MM made substantial contribution to conception and design and drafted the article.
FKC performed acquisition of data and revised the article critically for important intellectual content.
ZS made substantial contribution to interpretation of the data and revised the article critically for important intellectual content.
All authors read and approved the final manuscript.
Each author acknowledges that this final version was read and approved.
ETHIC STATEMENT BY ALL AUTHORS
This study was conducted with approval from the Institutional Review Board (or its equivalent) of all the institutions associated with this study as applicable.
Authors take responsibility to maintain relevant documentation in this respect.
LIST OF ABBREVIATIONS (In alphabetic order)
NOS - Not otherwise specified.
EDITORIAL/PEER-REVIEW STATEMENT
To ensure the integrity and highest quality of CytoJournal publications, the review process of this manuscript was conducted under a double-blind model (authors are blinded for reviewers and vice versa) through automatic online system.
REFERENCES
- Frozen section use in the diagnosis of ovarian pathology. In: Wilkinson N, ed. Pathology of the Ovary, Fallopian Tube and Peritoneum, Essentials of Diagnostic Gynecological Pathology. London: Springer Verlag; 2014. p. :133-48.
- [Google Scholar]
- Value of cytology in the intraoperative assessment of ovarian tumors: A review of 402 cases and comparison with frozen section diagnosis. Cancer Cytopathol. 2010;118:127-36.
- [Google Scholar]
- Intra-operative frozen section consultation: Concepts, applications and limitations. Malays J Med Sci. 2006;13:4-12.
- [Google Scholar]
- Role of intra-operative cytology in the diagnosis of ovarian neoplasm's. Int J Sci Stud. 2015;3:72-5.
- [Google Scholar]
- Useful aspects of diagnosis of imprint cytology in intraoperative consultation of ovarian tumors: Comparison between imprint cytology and frozen sections. Diagn Cytopathol. 2018;46:28-34.
- [Google Scholar]
- Comparative study between intraoperative frozen section and scrape smear cytology in the diagnosis of ovarian neoplasm. Open J Obstet Gynecol. 2015;5:28-35.
- [Google Scholar]
- The diagnostic utility of intraoperative cytology in the management of ovarian tumours. J Clin Diagn Res. 2013;7:1047-50.
- [Google Scholar]
- Role of intraoperative imprint cytology in diagnosis of suspected ovarian neoplasms. Asian Pac J Cancer Prev. 2010;11:1389-91.
- [Google Scholar]
- Contribution of intraoperative cytology to the diagnosis of ovarian lesions. Acta Cytol. 2011;55:85-91.
- [Google Scholar]
- The combined use of cytological imprint and frozen section in the intraoperative diagnosis of ovarian tumors. Int J Gynaecol Obstet. 1990;31:43-6.
- [Google Scholar]
- Value of cytology as an adjunctive intraoperative diagnostic method. An audit of 2,250 consecutive cases. Acta Cytol. 1997;41:1489-96.
- [Google Scholar]
- Usefulness of intraoperative imprint cytology in ovarian germ cell tumors. Acta Cytol. 2013;57:171-6.
- [Google Scholar]
- Imprint cytology versus frozen section analysis for intraoperative assessment of sentinel lymph node in breast cancer. Breast Cancer (Dove Med Press). 2017;9:325-30.
- [Google Scholar]
- Intraoperative diagnosis of central nervous system lesions: Comparison of squash smear, touch imprint, and frozen section. J Cytol. 2015;32:153-8.
- [Google Scholar]








