Translate this page into:
Diagnosis of pulmonary hydatid disease presenting with solid nodule and mimicking malignancy by fine needle aspiration cytology
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
To the Editor,
Hydatid disease (HD) is caused by Echinococcus granulosus, endemic in the cattle- and sheep-raising regions of the underdeveloped and developed world.[12]
The prevalence is rather high in several countries of the Mediterranean region, mainly in pastoral areas where the dog-sheep cycle of the parasite prevails.[3]
It also remains a health problem in Turkey, mainly in the rural areas of the eastern part of the country.[4]
Hydatid disease predominantly affects the liver and lungs. The relatively rare anatomic locations are the central nervous system, muscles, subcutaneous tissue, kidneys, bones, and body cavities.[1]
Pulmonary HD can be diagnosed by clinical and radiological findings, and serological analysis. However, old, arrested forms of the infection presenting with an organized, solid, atypical pulmonary nodule may mimic lung cancer.[5] Fine needle aspiration cytology (FNAC) can be a useful tool in the differential diagnosis.[6]
We report a case of pulmonary hydatid cyst presenting with a solid and solitary nodule, clinically and radiologically suspicious for malignancy, diagnosed by FNAC.
A 52-year-old female patient presented with a history of dyspnea and cough. Computed tomography (CT) revealed a solid nodular lesion, with a 2 cm diameter, in the apicoposterior segment of the upper lobe of the left lung [Figure 1].
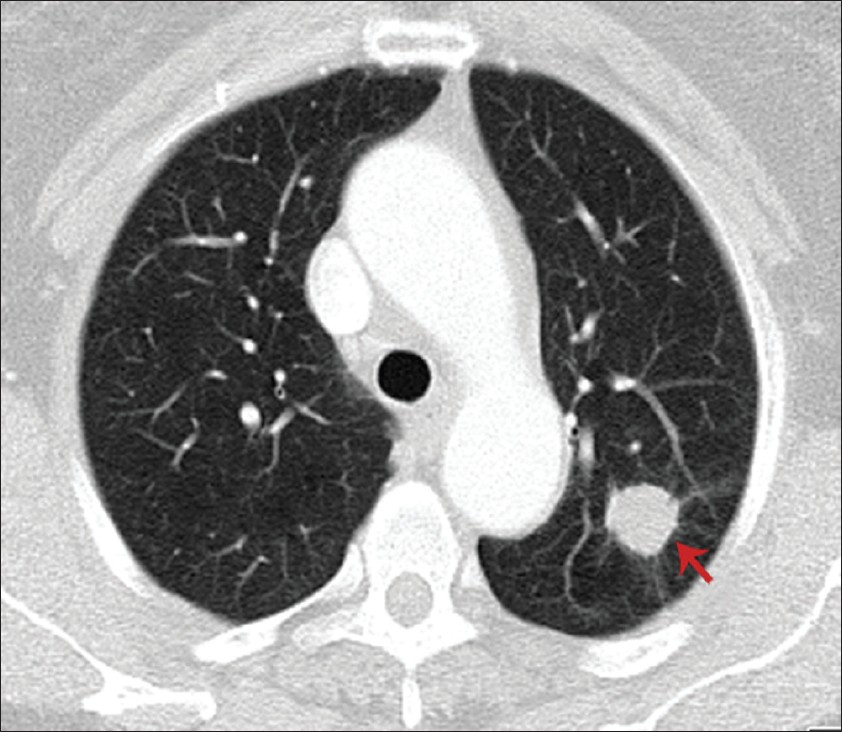
- Computed tomography image showing a nodular lesion (red arrow), 2 cm in diameter, in the apicoposterior segment of the upper lobe of the left lung
A clinical and radiological diagnosis of lung malignancy was rendered, and subsequently a CT-guided transthoracic FNAC was done.
CYTOMORPHOLOGICAL FEATURES
Direct air-dried smears from the aspirated material were stained with May-Grünwald-Giemsa (MGG) , and alcohol-fixed smears were stained with the Papanicolaou stain and hematoxylin and eosin.
The cytological smears showed laminated cyst wall particules (cuticula) and plenty of pathogonomic hooklets in the backgound of the necrotic debri, with inflammatory cell reaction in the form of neutrophils, foreign body giant cells, as well as hemosiderin-laden alveolar macrophages, and rective alveolar epithelial cells [Figures 2–5]. No scolices were seen, probably due to the chronicity of the lesion.
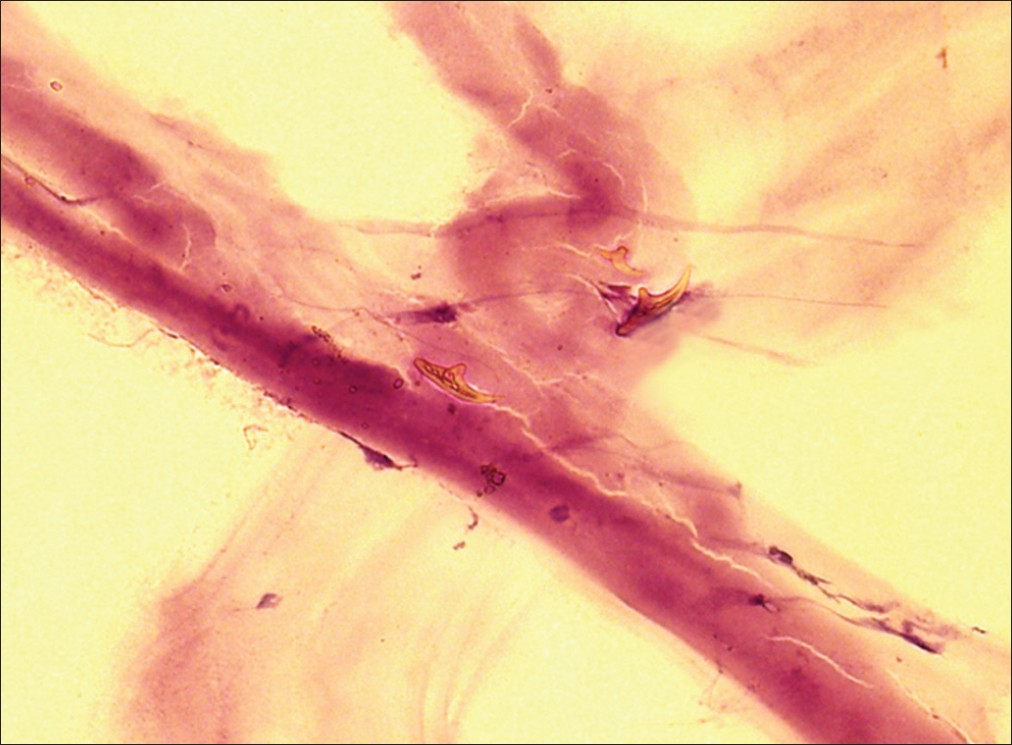
- Amorphous acellular laminated membrane (cuticula) with a few hooklets (H and E stain, ×400)
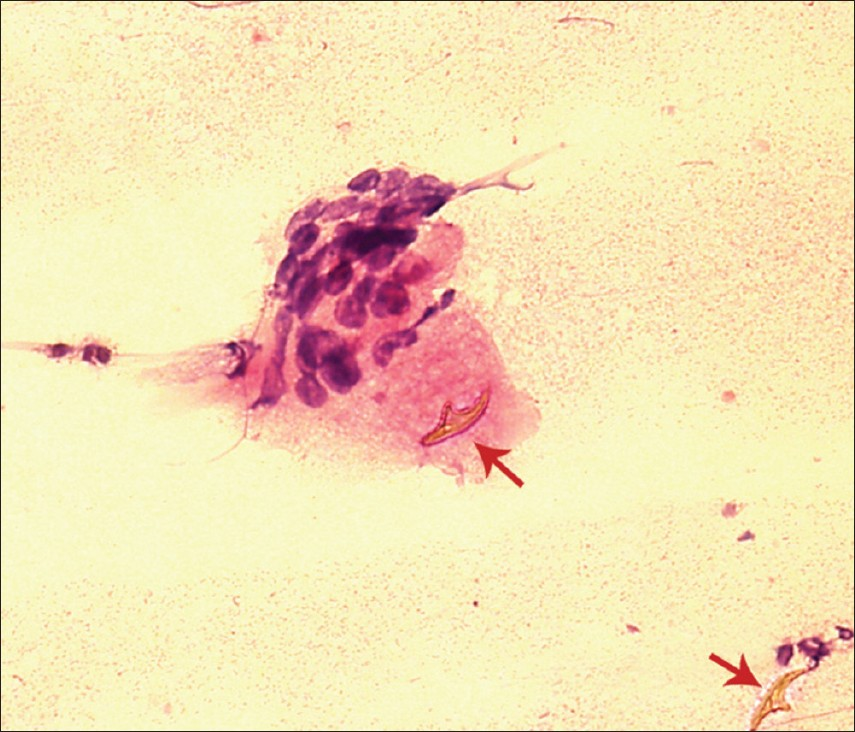
- A foreign body giant cell neighboring a hooklet and another hooklet in the lower right corner (red arrow) (H and E stain, ×400)
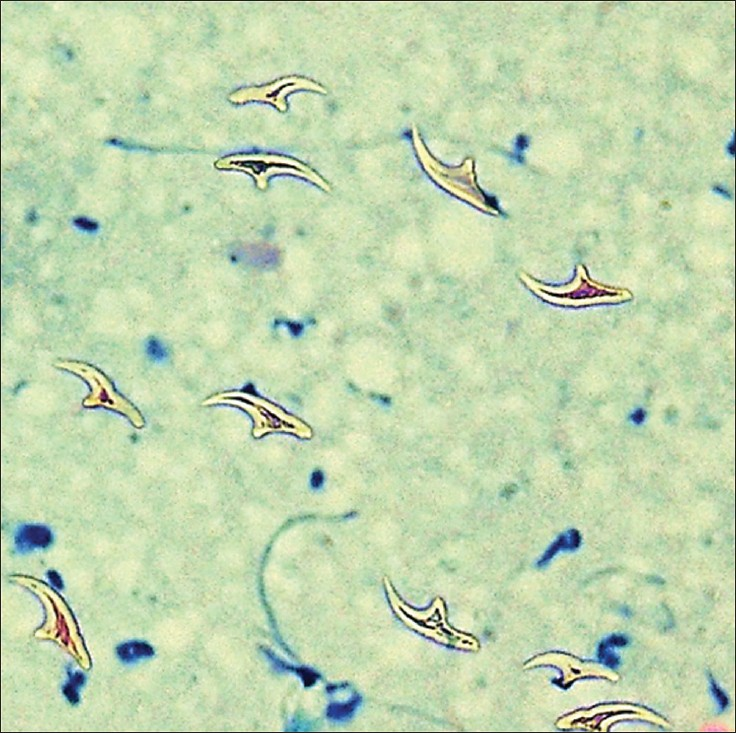
- A large group of free hooklets (MGG, ×400)
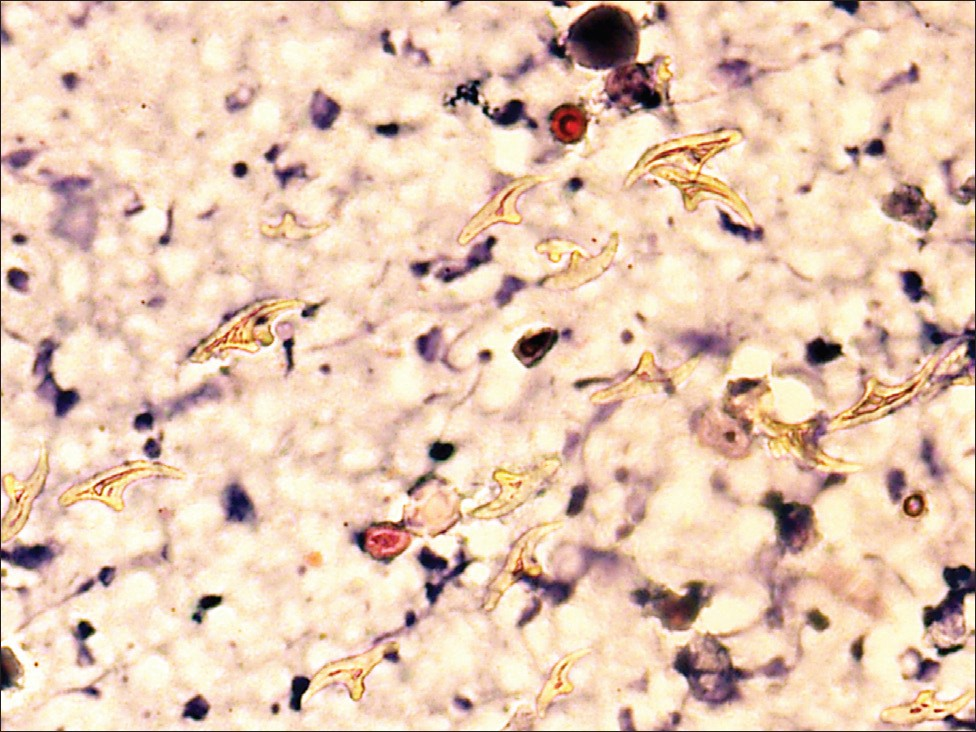
- Numerous free hooklets in the inflammatory background (H and E stain, ×400)
These findings were reported as ‘consistent with organized hydatid cyst’. Serological backup analysis was suggested. Subsequently, an echinococcosis Eliza IgG test was carried out and reported to be positive.
Following the cytodiagnosis, a radiological search revealed no other organ involvement. On consultation with ‘the Faculty Thorax Council’ consisting of specialist physicians from the Departments of Pathology, Radiology, Chest Diseases, Thoracic Surgery, and Oncology, it was decided that it was an organized and old solitary hydatid lesion, and a follow-up was advised to the patient without any medical or surgical treatment.
One year later a control CT scan was carried out , at the time of writing this report, and it showed no significant change in the lesion.
Hydatid disease is a chronic parasitic zoonotic infection in humans,which is transmitted between dogs and domestic livestock, particularly sheep.[2] It is still an important health problem not only in underdeveloping and developing countries, but also in industrialized countries, particularly in rural areas and / or among immigrant population from endemic countries.[1]
The lungs are the second-most common site of involvement after the liver. In fact, the diagnosis of pulmonary HD is based on clinical and radiological findings, and serological analysis (echinococcosis Eliza IgG test). FNAC is generally not preferred, and even regarded as contraindicated , due to fear of an untoward allergic reaction and dissemination following the procedure unless the presentation of the disease is atypical.[6–9]
Most of the patients with pulmonary HD are asymptomatic, but depending on the localization and the size it can produce some nonspecific symptoms, such as, cough, chest pain, and hemoptysis.[10] Unless the cysts are ruptured, the disease cannot cause systemic manifestations like fever, fatigue, and weight loss.
Old and organized forms of pulmonary infection may present with a solid and solitary nodule, which may clinically and radiologically mimic malignancy like in our case. In this situation, FNAC can be considered in the differential diagnosis.
Diagnostic cytomorphological features of HD include laminated cyst wall fragments (also called cuticula), scolices, and hooklets. Identification of hooklets is regarded pathogonomonic, and observation of laminated membranes by itself is a presumptive finding in the cytodiagnosis of HD.[11]
An acompanying infiltrate of inflammatory cell reaction with necrotic debri, foreign body giant cells, hemosiderin-laden alveolar macrophages are also seen in the background, but this infiltation by itself is not diagnostic.[8] These findings were present in our case, except scolices. The identification of scolices assumes more difficulty in old, arrested infections, when the outer layer of the cyst has been replaced by cellular inflammatory response and nonspecific collagenous tissue.[12]
Hydatid disease is endemic mainly in the rural areas of the eastern part of Turkey. In the western parts of the country, including the province (Kocaeli) neighboring Istanbul, where our medical faculty is located, the disease is encountered sporadically, mostly among the people who have migrated from the endemic areas, as it was in our case.
Fine needle aspiration cytology is a useful, rapid, and diagnostic technique for the diagnosis of an organized form of pulmonary HD, clinically mimicking malignancy. No post aspiration adverse reactions were reported in the FNAC of such cases.[7–91113]
First choice of treatment of pulmonary HD is surgery.[14] Medical treatment is an alternative to surgery where a surgical approach is not recommended in risk patients, and in cases with small and multiple lesions.[15] In our case, follow-up was preferred, because the lesion was old, arrested, and undersymptomatic.
On the other hand, one should bear in mind the possibility that carcinoma may rarely have clinical, radiological, and serological features, similar to those of a HD. Singh N, et al. reported a case of a large cell type lung carcinoma mimicking pulmonary HD, with a positive serological test for Echinococcus granulosus.[16] FNAC was not applied in this case, and the diagnosis of carcinoma was rendered histopathologically on the surgical specimen. The possible antigenic similarity between lung carcinoma and HD was also reported.[17] Literature screening revealed some cases of malignancy in the liver mimicking HD,[18–21] as well as occasional cases of carcinoma associated with HD.[22–25] The diagnosis of malignancy was confirmed by FNAC in the case with reference number 21, which was a case of undiffentiated embryonal sarcoma with atypical imaging features suggestive of HD, even though hydatid serology was negative. There was no record about the usage of FNAC in other cases.
In conclusion, in this report, our primary aim was to present the demonstative cytomorphological features of HD, and we also suggested that HD should be included in the differential diagnosis, in patients with solid pulmonary nodules, in the nonendemic regions of the endemic countries as well as in nonendemic countries having immigrant populations from endemic countries. In this case, the application of FNAC could be considered as a useful diagnostic method.
COMPETING INTEREST STATEMENT BY ALL AUTHORS
The author(s) declare that they do not have competing commercial interests.
AUTHORSHIP STATEMENT BY ALL AUTHORS
All authors of this article declare that they qualify for authorship as defined by ICMJE. All authors are responsible for the conception of this study, have participated in its design and coordination, and helped to draft the manuscript. All authors have read and approved the final manuscript.
ETHICS STATEMENT BY ALL AUTHORS
As this is a case report in the form of a letter without patient identifiers, approval from the Institutional Review Board (IRB) is not required.
EDITORIAL / PEER-REVIEW STATEMENT
To ensure the integrity and highest quality of CytoJournal publications, the review process of this manuscript was conducted under a double blind model (authors are blinded for reviewers and vice versa) through automatic online system.
Available FREE in open access from: http://www.cytojournal.com/text.asp?2012/9/1/13/95832.
REFERENCES
- Epidemiology, clinical manifestations and diagnosis of zoonotic cestode infections: an update. Parasitol Res. 2003;91:412-38.
- [Google Scholar]
- Control of cystic echinococcosis / hydatidosis: 1863-2002. Adv Parasitol. 2006;61:443-508.
- [Google Scholar]
- Echinococcosis / hydatidosis: a severe threat in Mediterranean countries. Vet Parasitol. 2010;174:2-11.
- [Google Scholar]
- Epidemiological survey and molecular characterization of Echinococcus granulosus in cattle in an endemic area of eastern Turkey. Vet Parasitol. 2010;172:347-9.
- [Google Scholar]
- Three atypical pulmonary hydatidosis lesions mimicking bronchial cancer from Turkey. New Microbiol. 2009;32:229-33.
- [Google Scholar]
- Cytodiagnosis of hydatid disease with Horner's syndrome: a case report. Acta Cytol. 2001;45:784-8.
- [Google Scholar]
- Echnicoccosis (hydatid disease) in Missouri: diagnosis by fine-needle aspiration of a lung cyst. Diagn Cytopathol. 1991;7:527-31.
- [Google Scholar]
- Ultrasound guided fine-needle aspiration cytology: diagnosis of hydatid disease of the abdomen and thorax. Diagn Cytopathol. 1995;12:173-6.
- [Google Scholar]
- Diagnosis of hydatid disease of abdomen and thorax by ultrasound guided fine needle aspiration cytology. Indian J Pathol Microbiol. 1999;42:155-6.
- [Google Scholar]
- Hydatid cyst disease of the lung as an unusual cause of massive hemoptysis: a case report. J Med Case Reports. 2009;3:21.
- [Google Scholar]
- Role of fine-needle biopsy in the diagnosis of hydatid cyst. Diagn Cytopathol. 1995;13:229-32.
- [Google Scholar]
- Repeated unintentional transthroracic needle aspiration of a pulmonary hydatid cyst. Scand J Infect Dis. 2001;33:941-2.
- [Google Scholar]
- Lung carcinoma mimicking hydatid cyst: A case report and review of the literature. Med Oncol. 2009;26:424-8.
- [Google Scholar]
- Possible antigenic similarity between pulmonary carcinoma and cysts of Echinococcus granulosus. Br Med J. 1979;1:1463-4.
- [Google Scholar]
- Rim calcification in primary liver cell carcinoma mimicking hydatid disease. Gut. 1994;35:567-8.
- [Google Scholar]
- Primary biliary cystadenocarcinoma perforating the duodenum and left intrahepatic biliary tree-mimicking a hydatid cyst. Liver. 1999;19:39-41.
- [Google Scholar]
- Primary biliary cystadenocarcinoma mimicking a complicated hydatid cyst. Chirurgia (Bucur). 2010;105:249-51.
- [Google Scholar]
- Undifferentiated embryonal sarcoma of liver in an adult masquerading as complicated hydatid cyst. Ann Hepatol. 2011;10:81-3.
- [Google Scholar]
- Hydatid cyst and renal adenocarcinoma: an exceptional association. Actas Urol Esp. 1994;18:58-63.
- [Google Scholar]
- Hydatid disease of the liver and associated hepatocellular carcinoma. Clin Gastroenterol Hepatol. 2005;3:35.
- [Google Scholar]
- Hepatocellular carcinoma complicated with echinococcal cyst of the liver. Khirurgiia (Sofiia). 2010;4-5:49-50.
- [Google Scholar]







