Translate this page into:
The value of preoperative ultrasound guided fine-needle aspiration cytology of radiologically suspicious axillary lymph nodes in breast cancer
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Preoperative ultrasound (US) and eventually US-guided fine-needle aspiration cytology (FNAC) of suspicious axillary lymph nodes (ALN) is a standard procedure in the work-up of suspicious breast lesions. Preoperative US FNAC may prevent sentinel node biopsy (SNB) procedure in 24-30% of patients with early stage breast carcinoma. The aim of this study was to evaluate the institutional results of this preoperative diagnostic procedure.
Materials and Methods:
A total of 182 cases of preoperative FNAC of suspicious ALN where retrieved from the pathology files. The results were compared with the final histology and staging. False negative (FN) FNAC cases were reviewed and possibly missed metastatic cases (2) were immunostained with the epithelial marker AE1/AE3.
Results:
There were no false positives, whereas 16 cases were FN. In all but one case the FN's represented sampling error. Half of the 16 FN cases in this series were macrometastases.
Discussion:
About 83% of the preoperatively aspirated cases were N+, indicating that a radiologically suspicious ALN has a very high risk of being metastatic. Preoperative US guided FNAC from radiologically suspicious ALN is highly efficient in detecting metastases. Depending on national guidelines, a preoperative, positive ALN FNAC might help to stratify the patients as to SNB and/or ALN dissection.
Keywords
Axillary lymph node
fine needle aspiration
sentinel node biopsy
ultrasound
INTRODUCTION
As one of the first hospitals in Norway, Oslo University Hospital (OUS), Ullevaal introduced sentinel node biopsy (SNB) as a routine method in March 2000. The institutional sentinel node (SN) positivity rate is 24%.[1]
Preoperative ultrasound (US) - guided fine needle aspiration cytology (FNAC) of radiologically suspicious axillary lymph nodes (ALN) emerged after the onset of the surgical SNB procedure. Preoperative US FNAC may prevent SNB procedure in 24-30% of patients with early stage breast carcinoma.[2345]
Ultrasound examination of both axillae is standard procedure when the breast radiologist finds a malignant or suspicious lesion in the breast. A cortical ALN thickness >2.5 mm is considered indication for US FNAC.[6] Sampling of the suspicious ALN's is done by a radiologist, whereas the attending pathologist do a rapid on site evaluation to assess the adequacy and give a preliminary diagnosis.
The aim of this study was to evaluate the institutional results of this preoperative diagnostic procedure.
MATERIALS AND METHODS
The files at the Department of Pathology, OUS, Ullevaal were searched for cytological cases with a T-code of ALN and procedure (P) code for US guided FNAC. SN diagnostics began in 2000, and the search included the years 2000-2011. Metastases from other primaries, metastases diagnoses after primary treatment for breast cancer, malignant lymphomas and all other findings not related to the work-up of a primary breast malignancy were excluded.
Air-dried and Diff-Quick stained smears were used for rapid assessment.
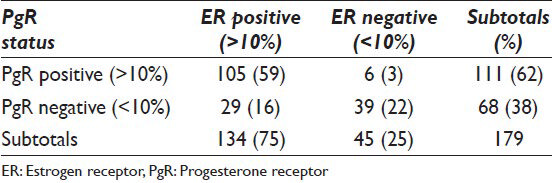
One hundred eight two cases were included in the study. TNM, subtype, grading,[7] tumor size, estrogen receptor (ER), progesterone receptors (PgR), HER-2, Ki-67 (testing for Ki-67 started in 2009), age and SN data were extracted from the pathology files of the department.
Estrogen receptor/PgR was registered as positive when >10% of the tumor cell nuclei were positive. National guidelines for ER positivity changed during the period the data for this study was collected. From 2011 >1% was considered positive according to the new guidelines. In order to have only one cut off for ER positivity, 10% was used through the whole study period. HER-2 was registered as positive when immunohistochemical expression was 3+ or when gene amplification with a ratio >2 had been found. Ki-67 expression was registered as <15% (low expression), 15-30% (intermediate expression) and >30% (high expression) according to national guidelines.[8]
All US FNAC cases that turned out to be false negative (FN) were morphologically reviewed. Slides with eventual suspicious groups or single cells were immunocytochemically (ICC) restained with an AE1/AE3 antibody.[9]
Cases where US FNAC was concordant with final histology were not reviewed.
RESULTS
The mean age of the women was 58 years (23-91). 179 tumors were invasive whereas 3 were pure ductal carcinoma in situ (DCIS) grade 3. Tumor size for invasive lesions varied from 2 mm to 100 mm, with a mean of 30.5 mm. The in situ lesions had extensions from 70 mm to 100 mm, with a mean of 83 mm (median = 80 mm). Axillary metastasis was diagnosed preoperatively in 133 cases (74%). A total of 151 cases were N+ (pN1 = 84, pN2 = 35, pN3 = 19 and pNx = 13) (83%) and 31 were pN0 (17%).
Overview of TNM, invasive subtypes, ER/PgR, HER-2 and Ki-67 status of invasive cases are shown in Tables 1 and 2. Ki-67 had been done in 72 of the cases.

In 13 cases the patient had received preoperative adjuvant treatment and one or more ALN showed fibrosis, but no rest of vital carcinoma cells. These had all been positive on US FNAC before treatment. The fibrosis was evaluated as a complete treatment response in primarily metastatic ALN and the patient as an N +.
All three pure DCIS had negative US FNAC and negative SN. SNB was done on all high-grade DCIS until 2010. Overview of FN US FNAC versus subtypes of invasive carcinoma and metastatic size is shown in Table 3.

There was no false positive US FNAC (specificity 100%; PPV 100%) evaluated against final histology after ALN dissection (ALND). The cytological material was unsatisfactory/insufficient in two cases. One of these had a negative SN and the other had a 4 mm metastasis in the SN.
For unknown reasons, SNB was omitted in 8 cases with negative US FNAC. Two of these were N+, whereas 6 were N0.
Sentinel node biopsy was done in 39 women. In an additional case, the SN was not found. Overview of US FNAC, SN and tumor subtypes are shown in Table 4.
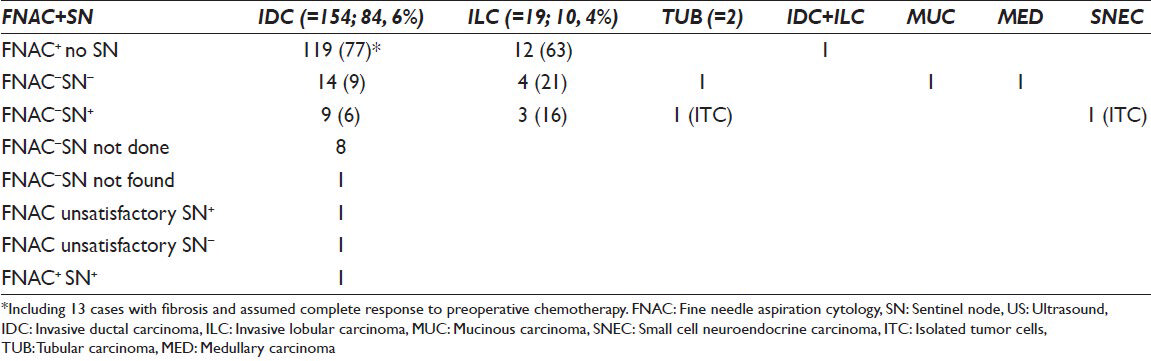
Sentinel node was positive in 17 women (17/39 = 43.6%) with a preoperative US FNAC, including one case that had been diagnosed as positive for malignancy. The size of SN metastases was 0.1-12 mm (mean 5.7 mm), including 2 ITC (0.1 mm and 0.18 mm) and 2 micrometastases (1.5 mm and 2 mm). Thirteen were macrometastases (76.5%).
There were 16 FN US FNAC (8.8%). The rate of FN was higher for ILC (16%) than for invasive ductal carcinoma (IDC) (6%). 14/16 smears were morphologically negative on review. In one case, suspicious groups were found in one of two smears. ICC restaining with AE1/AE3 was done on the suspicious smear and was positive [Figure 1]. The sensitivity of preoperative ALN FNAC was 89% and negative predictive value (NPV) was 66%.

- Case with false negative fine needle aspiration cytology of axillary lymph nodes, ultrasound image (a). Smear 1 from case showing lymphoid cells only (Giemsa, ×400) (b). Smear 2 from case showing groups of cells originally interpreted as aggregates of lymphoid cells (Giemsa, ×400) (c and d). Cells groups positive for the epithelial marker consistent with metastatic carcinoma (Immunocytochemically AE1/AE3 staining of smear 2 × 400) (f). Sentinel node frozen section showing axillary lymph nodes with macrometastasis (H and E, ×100) (g) Parafin embedded rest of sentinel node after frozen section showing metastatic carcinoma cells on large magnification (H and E, ×400) (h)
DISCUSSION
Ultrasound FNAC is a rapid, cheap and safe method for preoperative assessment of ALN. In accordance with our results, false positives are virtually nonexistent with reported specificities close to 100%.[10] A recent meta-analysis found an overall sensitivity and specificity of respectively 79.6% and 98.3% as well as a positive predictive value of 97.1%.[11] According to Jing et al.[12] liquid-based preparation of ALN aspirates yield similar results with a reported sensitivity and specificity of 77.5% and 100%, respectively, as well as an NPV of 53.7% and a nondiagnostic rate of 8%.
The guidelines may not be identical in all countries, but if the national guidelines according to preoperative clinical data recommend ALND, it is safe to do so without previous SNB when a preoperative cytological diagnosis of metastatic ALN has been given as specificity is close to 100%. This will save both operation theater time and resources for preoperative marking of SN.
Invasive ductal carcinoma was by far the most common subtype with 86% of cases, whereas 10% were lobular. ILC had a higher rate of FN (16%) and a higher rate of macrometastases (2/3 vs. 50%) compared with IDC. The number of ILC is small for definitive statistics, but the findings are similar to Jing et al.[12] indicating a lower sensitivity for metastatic ILC. Lobular carcinomas may show diffuse involvement in metastatic lymph nodes with a mainly single cell pattern in the aspirates and interpretation errors might occur.
Micrometastasis in the SN harbor a low risk for affection in other ALN's.[131415] Missed ITC and micrometastases are thus not important in the preoperative US FNAC of ALN. However, half of the 16 FN cases in this series were macrometastases [Table 3] and on review only one case revealed missed suspicious cells. At preoperative US FNAC, we do not know whether the aspirated node (s) are SN or not. It is quite possible that the FN cases that turned out to have macrometastases were not SN ALN, but secondary line negative ALN because the true SN were blocked by the macro metastasis.[16] Totally, 83% of the preoperatively aspirated cases were N+, indicating that in this context a radiologically suspicious ALN has a very high risk of being metastatic. If clinically indicated, woman with radiologically suspicious SLN and negative ALN FNAC, should undergo SNB.
Current ASCO guidelines for SNB[17] are shown in Table 5. Women with one to two metastatic SLNs planning to undergo breast-conserving surgery with whole-breast radiotherapy should not undergo ALND (in most cases). In these cases, a positive ALN FNAC might be considered a surrogate for an SLN, thus omitting the SNB procedure.
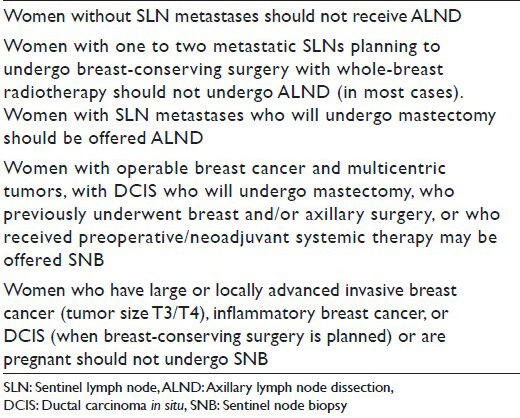
Women with SLN metastases who will undergo mastectomy should be offered ALND. According to our results, it is safe to do so on the basis of a preoperative ALN FNAC. Women with large or locally advanced invasive breast cancers (T3/T4), inflammatory breast cancer, or DCIS (when breast-conserving surgery is planned) or are pregnant should not undergo SNB. In this setting, a preoperative, positive ALN FNAC serve as a confirmation that axillary metastases are present.
CONCLUSION
Preoperative US guided FNAC from radiologically suspicious ALN is highly efficient in detecting metastases. The results will be of value in the preoperative work-up of the patient. Depending on national guidelines, a preoperative, positive ALN FNAC might help to stratify the patients as to SNB and/or ALND. In women with limited disease (stage 1-2) a positive, preoperative ALN FNAC might serve as a surrogate for SLN thus omitting the SNB procedure.
COMPETING INTERESTS
The authors declare that they have no competing interests.
AUTHORSHIP STATEMENT BY ALL AUTHORS
The requirements for authorship have been met
ETHICS STATEMENT BY ALL AUTHORS
The study has been approved by the institutional review board at Oslo University Hospital Ulleval.
EDITORIAL/PEER-REVIEW STATEMENT
To ensure the integrity and highest quality of CytoJournal publications, the review process of this manuscript was conducted under a double blind model (authors are blinded for reviewers and vice versa) through automatic online system.
REFERENCES
- Axillary recurrences after sentinel node surgery – Results over ten years in a university hospital. J Cancer Ther. 2012;3:846-52.
- [Google Scholar]
- Axillary lymph node echo-guided fine-needle aspiration cytology enables breast cancer patients to avoid a sentinel lymph node biopsy. Preliminary experience and a review of the literature. Surg Today. 2007;37:735-9.
- [Google Scholar]
- Reduction in the number of sentinel lymph node procedures by preoperative ultrasonography of the axilla in breast cancer. Eur J Cancer. 2003;39:1068-73.
- [Google Scholar]
- Prevention of futile sentinel node procedures in breast cancer: Ultrasonography of the axilla and fine-needle aspiration cytology are obligatory. Eur J Surg Oncol. 2008;34:497-500.
- [Google Scholar]
- A strategic approach to the evaluation of axillary lymph nodes in breast cancer patients: Analysis of 168 patients at a single institution. Am J Surg. 2007;194:524-6.
- [Google Scholar]
- Preoperative sonographic classification of axillary lymph nodes in patients with breast cancer: Node-to-node correlation with surgical histology and sentinel node biopsy results. AJR Am J Roentgenol. 2009;193:1731-7.
- [Google Scholar]
- Pathological prognostic factors in breast cancer. I. The value of histological grade in breast cancer: Experience from a large study with long-term follow-up. Histopathology. 1991;19:403-10.
- [Google Scholar]
- 2013. Available from: http://nbcg.no/behandlingsskjemaer
- Method development for DuoCISH HER-2 on FNAC material from breast carcinomas. Cytopathology. 2009;20(Suppl 1):110.
- [Google Scholar]
- Impact of preoperative ultrasonography and fine-needle aspiration of axillary lymph nodes on surgical management of primary breast cancer. Ann Surg Oncol. 2011;18:738-44.
- [Google Scholar]
- Preoperative ultrasound-guided needle biopsy of axillary nodes in invasive breast cancer: Meta-analysis of its accuracy and utility in staging the axilla. Ann Surg. 2011;254:243-51.
- [Google Scholar]
- Diagnostic value of fine needle aspirates processed by ThinPrep® for the assessment of axillary lymph node status in patients with invasive carcinoma of the breast. Cytopathology. 2013;24:372-6.
- [Google Scholar]
- Impact of micrometastases in the sentinel node of patients with invasive breast cancer. J Clin Oncol. 2009;27:4679-84.
- [Google Scholar]
- Sentinel lymph node dissection for breast cancer: Indications and outcomes. 2013. Available from: www.uptodate.com/contents/sentinel-lymph-node-dissection-for-breast-cancer-indications-and-outcomes
- [Google Scholar]
- Non sentinel node involvement prediction for sentinel node micrometastases in breast cancer: Nomogram validation and comparison with other models. Breast. 2012;21:204-9.
- [Google Scholar]
- Eight false negative sentinel node procedures in breast cancer: What went wrong? Eur J Surg Oncol. 2003;29:336-40.
- [Google Scholar]
- Sentinel lymph node biopsy for patients with early-stage breast cancer: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol. 2014;32:1365-83.
- [Google Scholar]








